The biggest difference between a midwife and an obstetrician really comes down to their philosophy of care. Midwives generally see birth as a natural, physiological process. They focus on holistic support with minimal intervention, especially for healthy, low-risk pregnancies. In contrast, obstetricians are medical doctors trained to manage the entire spectrum of pregnancy, from routine to high-risk, specializing in medical and surgical solutions when needed.
Understanding the Core Difference in Care
Choosing who will guide you through your pregnancy is a huge decision that really sets the tone for your entire journey. The choice often boils down to two incredible, highly qualified professionals: the midwife and the obstetrician. While both are dedicated to a healthy outcome for you and your baby, their approaches are shaped by very different training and philosophies.
An obstetrician, or OB/GYN, is a physician who has gone through medical school and then completed a specialized residency in obstetrics and gynecology. Their training is deeply rooted in medicine and surgery, making them the experts in handling complications, performing cesarean sections, and managing high-risk pregnancies. You'll almost always find them practicing in hospitals where advanced medical technology is right at their fingertips.
Midwives, on the other hand, are healthcare professionals who specialize in pregnancy, childbirth, and postpartum care with a focus on what's normal and natural. There are a few different types, and their care model is typically high-touch and low-tech. You can learn more about the distinctions in our detailed guide on Certified Nurse-Midwife vs. Certified Professional Midwife. They see birth as a physiological event, not primarily a medical one.
The fundamental distinction lies in their primary focus. Obstetricians are experts in managing pathology and complications, while midwives are experts in supporting the natural progression of pregnancy and birth.
This philosophical split between a midwife and an obstetrician influences everything, from how long your prenatal appointments are to the way labor is managed.
Midwife vs Obstetrician at a Glance
For a quick breakdown, this table offers a summary of the primary differences in philosophy, training, and typical patient focus between midwives and obstetricians.
| Aspect | Midwife | Obstetrician (OB/GYN) |
|---|---|---|
| Philosophy of Care | Views birth as a natural, physiological process. Focuses on holistic wellness and minimal intervention. | Views birth through a medical lens. Focuses on managing health and mitigating potential risks. |
| Typical Patient | Low-risk pregnancies. | Low-risk, high-risk, and complex pregnancies. |
| Training | Nursing or direct-entry midwifery programs, with a focus on physiological birth. | Medical school followed by a surgical residency in obstetrics and gynecology. |
| Birth Settings | Hospitals, birth centers, and homes. | Almost exclusively in hospitals. |
Ultimately, this table highlights how each provider is uniquely equipped to support different types of pregnancies and birth preferences.
Comparing Their Training Philosophies and Backgrounds
The paths to becoming a midwife or an obstetrician are worlds apart, and those differences really shape how each provider approaches your care. It’s the core distinction that influences everything from a routine prenatal check-up to the support you receive in the delivery room. One journey is steeped in a tradition of holistic, physiological support, while the other is built on a foundation of medical science and surgery.
Midwifery is one of the oldest health professions out there, with a history deeply rooted in community support and a profound trust in the natural process of birth. Back in the day, midwives were pillars of their communities. Interestingly, by the 17th century in England, midwives had surprisingly high literacy rates, a testament to their recognized and respected role long before modern medicine.
Midwifery Education and Certification
Today’s midwives follow rigorous, accredited programs that carry on this legacy. Their training is laser-focused on physiological birth, emotional wellness, and empowering the person giving birth. There are a few different types of midwives, and each has a specific training pathway.
- Certified Nurse-Midwives (CNMs) are registered nurses who’ve gone on to earn a graduate-level degree in midwifery. They’re certified by the American Midwifery Certification Board and can practice in all 50 states.
- Certified Midwives (CMs) complete a similar graduate program but often come from a health-related field other than nursing.
- Certified Professional Midwives (CPMs) specialize in out-of-hospital births, like at home or in birth centers. Their certification comes from the North American Registry of Midwives, and their training is often rooted in hands-on apprenticeships. If you're curious about this route, we have a great guide on how to become a direct-entry midwife.
This educational model positions midwives as true experts in normal, low-risk pregnancy and birth.
The Obstetrician's Medical Path
Obstetricians, on the other hand, are medical doctors. Their journey kicks off with four years of medical school, where they get a broad education in human anatomy, disease, and pharmacology. After that, they complete a tough, four-year residency in obstetrics and gynecology.
At its heart, an OB/GYN’s residency is all about surgical training and managing medical complications. They become specialists in spotting and treating problems, from pre-eclampsia to performing emergency C-sections.
This intensive training prepares them to handle virtually any scenario, including high-risk pregnancies, twins or triplets, and any emergency that might pop up during labor. To get a real sense of what they go through, you can look into their demanding OBGYN clerkship, which gives a glimpse into the rigor of their education. Once their residency is done, many become board-certified by the American Board of Obstetrics and Gynecology, which is a significant mark of distinction. Their expertise in pathology and surgery is exactly what makes them essential for complex pregnancies.
How Your Care Looks from Pregnancy to Postpartum
From that first prenatal visit to the final postpartum checkup, the day-to-day experience with a midwife versus an obstetrician can feel quite different. Each provider's approach shapes your journey, and understanding these nuances helps you picture what your pregnancy, birth, and early parenting phase might look like.
The difference often starts right from the first appointment. A visit with a midwife tends to be longer and feels distinctly personal. They dedicate a lot of time to discussing nutrition, your emotional well-being, and creating a detailed birth plan that truly reflects what you want.
Obstetricians are also incredibly thorough, but their appointments are often more clinically focused. The priority is on monitoring key health markers, going over test results, and identifying any potential risks that could come up.
Prenatal Care and Your Relationship with Your Provider
Building a relationship with your provider is a huge part of the experience, and the structure of prenatal care really influences how that connection develops.
With a midwife, you'll likely feel a deeper sense of partnership. Because their model allows for more time per visit, there's more space for questions and shared decision-making. This fosters a strong sense of trust and personal connection as you move through your pregnancy.
Obstetricians also build strong patient relationships, but the dynamic can feel different. Their main goal is to ensure medical safety and manage your health with precision. This means conversations might center more on clinical assessments and medical guidance, which provides a ton of reassurance, especially if you have any health concerns.
The core difference in prenatal care is often about time and focus. Midwifery appointments tend to be longer and more holistic, while OB appointments are efficient and medically centered. Both paths lead to excellent, safe care. They just take different routes to get there.
Labor, Delivery, and Postpartum Support
During labor, the contrast between a midwife and an OB becomes even clearer. Midwives are known for providing continuous, hands-on support. They encourage movement, suggest different laboring positions, and use natural comfort measures to help you progress.
An OB, on the other hand, coordinates with the entire hospital team to manage your labor. They are on hand to oversee everything and are ready to step in with any necessary medical interventions, like administering an epidural or performing a C-section if it becomes medically necessary.
Postpartum care also looks quite different. Midwifery care often extends well beyond the delivery room.
- Home Visits: Many midwives make home visits in the first few days or weeks to check on both you and the baby.
- Lactation Support: They are typically well-versed in breastfeeding and can provide hands-on lactation help.
- Mental Health: There is a strong focus on checking in on your emotional well-being and screening for postpartum mood disorders.
Obstetric care usually wraps up with a final office visit around six weeks postpartum. While this checkup is crucial for your physical recovery, ongoing support for things like lactation or mental health might require referrals to other specialists. For those wanting more comprehensive postpartum help, it’s worth exploring the ways a midwife supports you during the postpartum period. This comparison helps paint a clear picture of what your postpartum journey could look like.
Exploring Birth Settings and Intervention Rates
Your choice of provider is directly tied to where you can give birth. This is a huge decision, one that fundamentally shapes your experience and even influences the likelihood of certain medical interventions. The real difference between a midwife and an obstetrician often snaps into focus when you look at the environments they work in and the outcomes they typically see.
Obstetricians almost always practice in hospitals. That’s their turf. This setting guarantees immediate access to a full suite of medical technology, from continuous fetal monitoring to surgical suites for emergency C-sections. For anyone with a high-risk pregnancy, or for those who simply want the peace of mind that comes with having every medical and surgical tool on standby, a hospital is the standard and safest path.
Midwives, on the other hand, offer a lot more flexibility. You'll find them working across a whole spectrum of settings, including hospitals, dedicated birth centers, and private homes. This versatility is key to their model of care, allowing them to create an environment that supports natural labor with minimal interference, all tailored to what the birthing person wants.
Where You Can Give Birth
The setting you choose is more than just a location; it's a philosophy of care brought to life. Each option comes with a completely different set of tools, protocols, and overall vibe.
- Hospitals: The primary workplace for OB/GYNs and many Certified Nurse-Midwives (CNMs). Hospitals provide the highest level of medical care and are equipped for any and every complication.
- Birth Centers: These spots are usually staffed by midwives and offer a comfortable, almost home-like setting. They are designed specifically for low-risk pregnancies and serve as a perfect middle ground between a home and a hospital birth.
- Home Births: For those who want the ultimate control over their environment, a home birth with a qualified midwife is a beautiful option. If you're curious about this path, our guide on how to have a home birth has some really valuable insights.
Comparing Intervention Rates
When it comes to low-risk pregnancies, a solid body of evidence shows that midwife-led care is linked to lower rates of medical interventions. This isn't about one provider being "better" than another. It's simply because their training and care philosophies naturally lead to different ways of managing labor and delivery. The data really highlights this contrast.
Statistically, the difference in outcomes is pretty significant. One major comparative study found that labor induction happened in just 14.7% of women managed by midwives, compared to 20.4% with obstetricians. You can dive into the numbers yourself in the full analysis of midwifery versus obstetrical care.
The data is even more striking for first-time mothers under midwifery care. They were found to be 74% less likely to have labor induced and 75% less likely to have an epidural, all without compromising the safety of the baby or parent.
These numbers really reflect the midwifery model's core principle: patience with the natural rhythm of labor. By focusing on comfort measures and continuous, hands-on support, midwives can often help labor progress without needing interventions like Pitocin or an epidural. An obstetrician, trained to manage and mitigate risk, might suggest interventions sooner to ensure a predictable and medically controlled outcome, a valid and often necessary approach in many situations.
What Global Healthcare Models Can Teach Us
Looking at how other countries handle pregnancy care really puts the midwife vs. obstetrician conversation into perspective. The American system isn't the only way to do things, and many other models show just how powerful a strong emphasis on midwifery can be. This global view helps clarify the unique, and vital, roles each provider can play.
In many European countries, midwives are the go-to providers for the vast majority of pregnancies. Obstetricians function more like specialists, stepping in only for high-risk situations or when complications pop up. This approach frames birth as a normal life event, not an automatic medical procedure.
The Midwife-Led Model in Practice
Countries like the Netherlands and Sweden are perfect examples of successful midwife-led care. In these places, a midwife is the first person you see when you're pregnant, and this care model is directly tied to some of the best maternal health statistics in the world. They consistently report lower C-section rates and higher satisfaction among birthing parents.
This model is built on a spirit of collaboration. If a pregnancy veers into complicated territory, the midwife seamlessly hands off care to an obstetrician, making sure the right level of medical expertise is always on deck. It's a system built on using the right tool for the right job.
A key takeaway from global models is that integrating midwives as primary care providers for low-risk pregnancies is a proven strategy for improving maternal and infant outcomes. It balances holistic support with specialized medical oversight.
How the US Compares
The U.S. model is a world apart, typically defaulting to an obstetrician-led approach even for the most straightforward pregnancies. This has a direct impact on our maternal health statistics. The U.S. has about four midwives for every 1,000 live births, a stark contrast to France and Germany, where that number is over 25. This gap is reflected in our outcomes: the U.S. has one of the highest maternal mortality rates among wealthy nations, at 17.4 deaths per 100,000 live births. You can dig into these global midwifery statistics on statista.com.
In contrast, countries with robust midwifery systems see far better results. These healthcare models prove that when midwives and OBs work together, they create a powerful balance of personalized support and expert medical care. This kind of integration is exactly what many families are looking for, and financial access is a huge piece of that puzzle. For example, understanding Medicaid coverage for birth support can be a critical step in building your dream team. The evidence from around the world is clear: greater integration of midwifery care could be a key to turning the tide on maternal health in the U.S.
How to Make the Right Choice for Your Birth
So, how do you decide which path is right for you? Thinking about the difference between a midwife and an obstetrician really comes down to a few key things: your personal health needs, your core values, and the kind of birth experience you're hoping for. It's less about which provider is "better" and much more about finding the right fit for your unique situation.
An obstetrician is almost always the clear choice if your pregnancy is considered high-risk. This includes situations like carrying twins or other multiples, having a pre-existing medical condition like high blood pressure or diabetes, or if you already know you want a scheduled C-section. In these cases, their surgical training and expertise are exactly what you need.
On the other hand, a midwife is a fantastic option for a healthy, low-risk pregnancy. If your main goals are a low-intervention birth with continuous, hands-on support, a midwife's philosophy of care will likely be a perfect match.
Considering a Hybrid Model
You don't always have to pick just one. In fact, many families are discovering the sweet spot in a collaborative care or hybrid model.
A hybrid approach offers the best of both worlds. It combines the personal, hands-on support of a midwife with the medical expertise of an obstetrician, ensuring you’re covered no matter what happens.
This decision tree can help you visualize which primary care model aligns with your pregnancy's risk level.
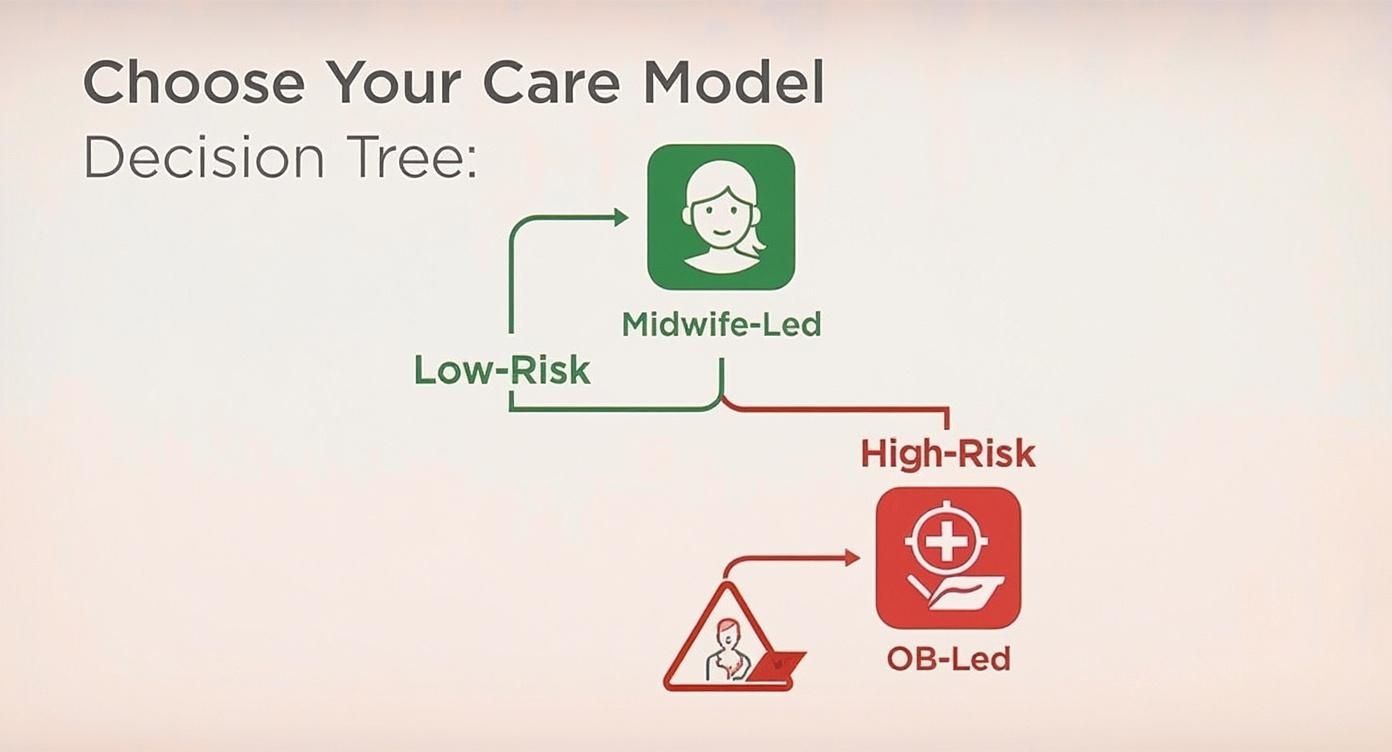
As the diagram shows, the paths are pretty clear, guiding low-risk pregnancies toward midwife-led care and high-risk ones toward an OB.
For instance, you might see a midwife for all of your prenatal appointments and then deliver in a hospital where an OB is on call just in case a complication arises. Another popular setup is choosing a practice where midwives and obstetricians work side-by-side, managing your care as a unified team. This provides a safety net that many families find incredibly reassuring.
Questions to Ask Your Potential Provider
To find your perfect match, it’s a great idea to interview a few potential providers. Think of it like a first date. You're looking for a connection. Here are a few questions to get the conversation started.
- What is your philosophy on birth? This is a big one. It helps you understand if their general approach vibes with your own.
- What happens if my low-risk pregnancy becomes high-risk? It's so important to know their process for transferring care if circumstances change.
- What is your C-section rate for low-risk patients? This number can give you a clue about their intervention style and how they manage labor.
- How do you support my birth plan? You want a provider who respects your wishes and truly believes in shared decision-making, not just someone who nods along.
Answering Your Lingering Questions
When you're weighing the pros and cons of a midwife versus an obstetrician, a few practical questions always seem to pop up. Let's clear the air on some of the most common ones families ask about insurance, pain management, and what happens if things don't go according to plan.
Will My Insurance Cover a Midwife?
This is a big one, and the good news is, most insurance plans, including Medicaid, do cover care from Certified Nurse-Midwives (CNMs). Because they are licensed healthcare professionals, their services are typically billed just like a physician's.
Coverage for other types of midwives, however, can be a bit more varied. It's always a smart move to call your insurance provider directly and ask about your specific plan. A quick phone call can save you from any surprise bills down the road.
Can I Still Get an Epidural with a Midwife?
Yes, absolutely. A very common myth is that choosing a midwife means you have to commit to an unmedicated birth. That's simply not true.
If you are giving birth in a hospital with a midwife, an epidural is definitely an option for you. Midwives are there to support your birth plan, whatever that looks like. If pain relief is part of that plan, they will work directly with the hospital's anesthesiology team to make it happen. Their job is to honor your choices.
Choosing a midwife doesn't lock you out of pain relief options. In a hospital setting, midwives fully support the use of epidurals if that’s what the birthing person wants. It’s all about your comfort and your plan.
What if My Pregnancy Becomes High-Risk?
Midwives are expertly trained to monitor your health and spot the earliest signs of complications. If a low-risk pregnancy starts to show signs of becoming high-risk, they have a clear and established protocol.
This usually involves consulting with an obstetrician they partner with or, if necessary, smoothly transferring your care. This collaboration ensures you and your baby get the specialized medical attention you need, right when you need it.
Finding the perfect provider for your family’s journey can feel like a huge task. Bornbir simplifies the search by connecting you to a network of over 6,000 vetted midwives, doulas, and other birth professionals. You can easily compare providers and find your perfect match at https://www.bornbir.com.
