So, how long does postpartum bleeding last? The straightforward answer is that this bleeding, also called lochia, typically sticks around for four to six weeks. But it's not a constant, heavy flow for that entire time. It’s actually a gradual healing process with a few distinct phases.
Your Guide to the Postpartum Bleeding Timeline
 Welcome to your postpartum recovery. One of the first things you'll notice is the bleeding, which is a totally natural and necessary part of your body's healing journey after giving birth. This is simply your body’s way of clearing out the uterine lining that so wonderfully supported your baby for months.
Welcome to your postpartum recovery. One of the first things you'll notice is the bleeding, which is a totally natural and necessary part of your body's healing journey after giving birth. This is simply your body’s way of clearing out the uterine lining that so wonderfully supported your baby for months.
Think of it as your body's own internal cleanup crew. It starts out looking a lot like a heavy period, then gradually tapers off, changing color and consistency over the next several weeks.
Understanding the Stages
This transition from heavy bleeding to light spotting doesn't happen overnight. It unfolds in a few key stages, each with its own look and feel. Knowing what's coming can make the whole process feel much more manageable.
To make it easier to track, here's a simple breakdown of what to expect week by week.
The Stages of Postpartum Bleeding (Lochia)
| Stage & Timeline | What to Expect (Color & Flow) | Key Notes |
|---|---|---|
| Lochia Rubra (Days 1-4) | Bright red, heavy flow, similar to the heaviest days of your period. You might see some small clots. | This is the most intense phase. Your body is shedding the thickest part of the uterine lining. |
| Lochia Serosa (Days 4-10) | The flow lightens up, turning a pinkish or brownish color. It becomes much more watery in consistency. | A good sign that healing is well underway. The color change means there's less fresh blood. |
| Lochia Alba (Up to 6 weeks) | The discharge becomes yellowish-white and is much lighter. This stage is often just spotting. | This is the final stage of the cleanup process as your body gets back to its pre-pregnancy state. |
Knowing what to expect can help you feel more prepared and in control during this phase of recovery, a period often called the fourth trimester. Understanding this timeline helps you recognize what's normal for your body's healing process and, just as importantly, when you might need to reach out for extra support from your healthcare provider.
Understanding Why Postpartum Bleeding Happens
To really get a handle on the question "how long does postpartum bleeding last?" it helps to understand what’s actually happening inside your body after birth. This discharge, officially called lochia, is so much more than just blood. It's your body's way of clearing out leftover blood, mucus, and tissue from the uterine lining that nourished your baby for nine whole months.
Think of it this way: your uterus built a cozy, fully furnished home for your baby. After your baby moves out, that home needs a serious deep clean. Lochia is your body's natural and incredibly efficient way of clearing everything out, allowing the uterus to shrink back to its pre-pregnancy size and get back to business as usual.
The Placenta and Uterine Healing
The main event that kicks off this whole process is the delivery of the placenta. Right after your baby is born, your body delivers the placenta, the amazing organ that connected you both. When it detaches from the uterine wall, it leaves behind a wound.
This placental site is like a large scrape inside your uterus, roughly the size of a dinner plate. Just like any wound, it needs time to heal, and the bleeding you experience is a direct result of this healing process. The open blood vessels at that spot are the source of the initial heavy, bright red bleeding.
Lochia is the body's method for healing and resetting the uterus. It’s a mix of blood, fluid, and tissue that your body no longer needs after pregnancy, and it's a clear sign that your recovery is underway.
As your uterus contracts and shrinks down over the next few weeks, it helps to clamp down on these blood vessels. This is why the bleeding gradually lessens and changes color over time. It’s a critical part of your recovery, managed by a team of hormones and your body's amazing ability to heal itself. You can find more details on this recovery phase by learning about the different aspects of perinatal care in our guide.
A Sign of Recovery, Not a Period
It’s really important to see this bleeding not as a period, but as a sign of healing. It’s a necessary function, no matter how you gave birth, vaginally or by C-section. Every single person who gives birth will experience it.
Understanding the "why" behind lochia can completely shift your perspective. Instead of seeing it as just another postpartum inconvenience, you can recognize it as a positive, productive part of your journey. Your body is doing exactly what it needs to do to recover from the massive job of growing and birthing a human.
A Week By Week Breakdown of Lochia
Postpartum bleeding, known as lochia, almost always follows a predictable pattern as your body heals itself after birth. While everyone’s timeline is a little different, knowing the typical stages can give you peace of mind and help you track your own recovery.
Think of it like a healing wound. It changes in color and consistency over time as it gets better. This is your body's visible sign that it's on the mend. Knowing what to expect can make you feel more in control and less worried about the changes you’re seeing.
Stage 1: Lochia Rubra (The First Few Days)
The first stage, lochia rubra, kicks off right after you give birth and usually lasts for about three to four days. This is when the bleeding is at its heaviest and most vibrant. Expect a flow that feels similar to the first couple of days of a very heavy period, with a dark or bright red color.
It's also completely normal to pass some small blood clots during this time, typically no larger than a quarter. This is just your body shedding the thickest part of the uterine lining and tissue from where the placenta was attached.
This visual shows how the postpartum bleeding process is tied directly to the birth of your baby and the subsequent healing of your uterus.
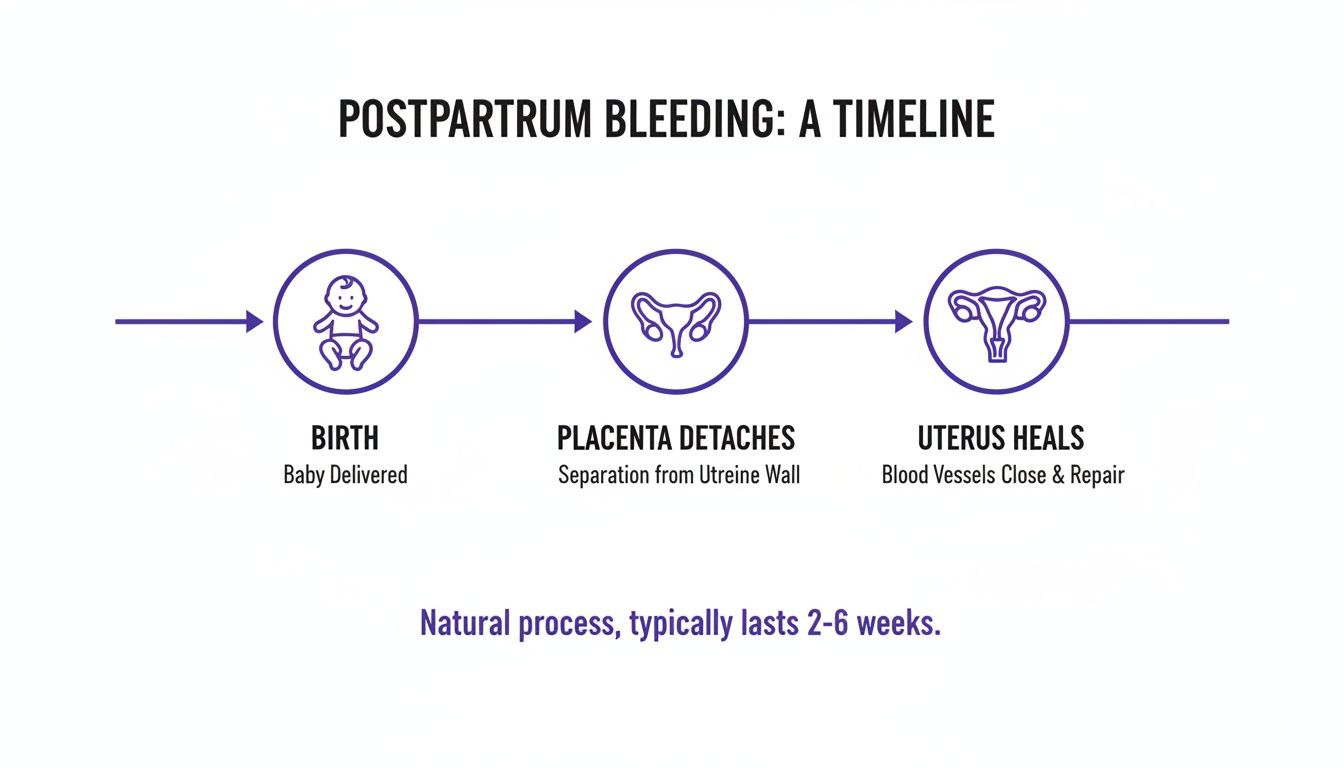 As the timeline shows, the bleeding is a direct result of the placenta detaching, which creates a wound inside your uterus that needs time to heal.
As the timeline shows, the bleeding is a direct result of the placenta detaching, which creates a wound inside your uterus that needs time to heal.
Stage 2: Lochia Serosa (The Transition Phase)
Around day four, you'll start to notice a change as you enter the second stage, known as lochia serosa. This phase lasts until about day ten to twelve and signals a real shift in your postpartum bleeding. The discharge will become much thinner and more watery.
The color will also change, moving from red to a pinkish or brownish hue. This is a fantastic sign that your uterus is healing well and there's much less fresh blood in the discharge. You will still need a pad, but the flow should be noticeably lighter than in those first few days.
This gradual lightening is exactly what you want to see. It shows your body is making steady progress. For extra support during this time, it can be helpful to know what a postpartum doula visit might look like.
Stage 3: Lochia Alba (The Final Weeks)
The final stage is called lochia alba, which means "white lochia." This phase can begin around day twelve and continue for several more weeks, sometimes right up to the six-week mark. At this point, the discharge changes to a yellowish-white color.
This discharge is made up mostly of white blood cells, mucus, and old uterine lining cells, with very little blood left. The flow will be much lighter, often just some spotting that might come and go. You’ll probably only need a thin panty liner for this stage.
This progression, from a heavy red flow to a scant yellowish-white discharge, is a key part of the healing process. For 80-90% of cases, this entire journey is wrapped up within six weeks. Knowing this helps families distinguish between a normal recovery and something that might need a doctor's attention.
Factors That Influence Your Bleeding Timeline
So, you've heard the standard four to six weeks answer for how long postpartum bleeding lasts, but your own journey might look a little different. It's not a one-size-fits-all experience. Several key things can speed up or slow down your body’s unique recovery process.
Think of it less like a fixed deadline on a calendar and more like a dynamic process. It’s shaped by how you gave birth, the choices you make postpartum, and your body’s individual healing rhythm. Understanding these factors can help you set realistic expectations and feel more in tune with your recovery.
Your Delivery Method Matters
The way your baby arrived plays a huge role in what to expect from postpartum bleeding. It’s probably one of the biggest variables that can change the length and intensity of your lochia.
- Vaginal Delivery: After a vaginal birth, it's common to have a longer and sometimes heavier bleeding duration. This is totally normal. Your uterus is left to shed its entire lining and heal the placental site on its own timeline.
- Cesarean Section (C-section): If you had a C-section, you might notice the bleeding is a bit lighter, especially in the first few days. That's because, during the procedure, the surgeon often manually clears out some of the uterine lining, giving your body a head start on the cleanup.
Even with a C-section, you will still go through all three stages of lochia. The internal healing is just as important as what's happening on the outside. If you want to learn more, check out our guide on how to properly care for a C-section incision.
How Breastfeeding Changes Things
Believe it or not, breastfeeding has a direct impact on your uterus and, by extension, your postpartum bleeding. When you nurse, your body releases the hormone oxytocin. This powerful hormone causes your uterus to contract, which you might feel as mild cramping, often called "afterpains."
These contractions are doing two important things. First, they can cause a temporary gush of blood during or right after a feeding session, which is completely normal. But second, those same contractions are helping your uterus shrink back to its pre-pregnancy size more efficiently. This can actually help the overall bleeding process wrap up a little faster.
Other Influential Factors
Beyond how you delivered and your feeding choices, a few other things can tweak your bleeding timeline. Your body’s recovery is a complex process with many moving parts.
It's so important to remember that every recovery is unique. Things like having multiples, your activity level, and even your personal health history all contribute to how long postpartum bleeding will last for you.
Here are some other things that can influence your lochia:
- Multiple Births: If you carried twins, triplets, or more, your uterus was stretched more and the placental site is larger. This can sometimes lead to a longer or heavier bleeding period as your body has a bit more healing to do.
- Your Activity Level: Getting back on your feet is great, but doing too much, too soon can sometimes cause your bleeding to temporarily increase or turn bright red again. This is your body’s not-so-subtle way of telling you to slow down and rest.
- Your Body’s Healing Pace: Just like some people bounce back from a cold faster than others, every person’s internal healing clock is different. Your body will take the time it needs, so try to be patient with the process.
Warning Signs to Watch For With Postpartum Bleeding
Knowing the typical timeline for postpartum bleeding is one thing, and it can bring a lot of peace of mind. But it's just as crucial to know what isn't typical so you can spot any red flags right away. While serious complications are rare, being informed means you can act quickly if something feels off.
Think of it like telling the difference between a normal rain shower and a sudden, intense storm. Most of what you'll go through is completely expected, but you also need to recognize the signs that mean it's time to seek shelter and call for help. Your body is smart, and it will give you clues when it needs medical attention.
When to Contact Your Doctor
Always, always trust your instincts. You know your body better than anyone else. If something doesn't feel right, it’s always best to reach out to your OB-GYN, midwife, or family doctor. Certain symptoms demand immediate attention, as they could signal a postpartum hemorrhage (PPH) or an infection.
Here are the key warning signs to keep on your radar:
- Extremely heavy bleeding. This is a big one. If you are soaking through more than one heavy-duty maternity pad in an hour, that's a red flag.
- Passing large blood clots. While small clots are normal in the first few days, consistently passing clots larger than a golf ball is a reason to call your provider.
- Bleeding that suddenly gets heavier again. If your flow had started to lighten up and then abruptly returns to a heavy, bright red flow, it’s time to check in.
- A foul-smelling discharge. Lochia has its own distinct, kind of musty odor, but it should never smell foul or fishy. That could point to an infection.
- Feeling dizzy, weak, or having a racing heart. These could be signs of significant blood loss and need to be addressed immediately.
Your recovery is just as important as your new baby’s health. Never hesitate to advocate for yourself. If something feels wrong, it is always better to be cautious and make the call.
It's helpful to understand that postpartum hemorrhage isn't the same as the longer lochia phase. Research shows the global prevalence of PPH is around 9.97%, with most cases happening right after delivery. The extended lochia phase that follows is a crucial monitoring period for any delayed issues. You can discover more research about postpartum health to feel more informed.
These guidelines aren't meant to cause alarm. They're here to empower you with knowledge so you can feel confident and in control during your recovery. Having this information helps you understand what's normal for the postpartum bleeding timeline and when it's time to get the right care. You might also be interested in learning about other ways to get help during this time through postpartum support services.
Practical Tips for Managing Postpartum Bleeding

Let's be real. Managing postpartum bleeding is a big part of your day-to-day for the first several weeks. Having the right supplies and a solid self-care plan can make a world of difference in how comfortable and in control you feel while your body heals.
Think of this time as your recovery bubble. Simple, practical steps can help you navigate it with more ease.
Choosing the Right Products
First things first: you'll want to stock up on the right supplies. In those early days, the pads you use for your regular period just aren't going to cut it. You need something way more absorbent.
Heavy-duty maternity pads are your best friend right after birth. Go ahead and grab a few packs before you even come home from the hospital. They’re longer, thicker, and designed for the heavy flow you'll experience initially. As the bleeding tapers off over the weeks, you can comfortably switch to regular maxi pads and, eventually, panty liners.
There are also a couple of things you absolutely need to avoid while you're healing.
- No tampons or menstrual cups. Your provider will give you the green light when it's safe, but for at least the first six weeks, don't insert anything into your vagina. These products can introduce bacteria into your healing uterus and seriously increase your risk of infection.
- Use a peri bottle. This little squirt bottle is a lifesaver. Fill it with warm water and use it to gently rinse yourself after you use the toilet. Wiping with dry paper can be really irritating on sore, sensitive skin, so this gentle cleansing is a game-changer. Just pat yourself dry afterward.
Self-Care for Comfort and Healing
Beyond just products, the way you care for your body is crucial for a smooth recovery. Your priorities should be rest, hydration, and gentle hygiene. It sounds simple, but it’s so important.
Rest is not a luxury right now; it’s a necessity. Lying down can help reduce the pressure on your pelvic floor and may even lessen your flow a bit. If you notice an increase in bleeding after being active, that's your body's not-so-subtle signal to take it easy.
Remember that your recovery is just as important as your new baby's needs. Prioritizing rest, staying hydrated with plenty of water, and maintaining gentle hygiene are fundamental to a smooth healing process.
Staying well-hydrated is also key to helping your body recover, and it’s especially important for milk production if you’re breastfeeding. And on a purely practical note, leaks happen. Knowing how to get rid of blood from sheets can be surprisingly helpful for keeping your space clean and comfortable while you rest.
Got Questions About Postpartum Bleeding? We Have Answers.
Navigating postpartum recovery means you'll probably have a lot of questions. Getting clear, straightforward answers can be a huge relief and help you feel more in tune with what your body is going through.
Let's walk through some of the most common questions about the postpartum bleeding timeline. Just remember, everyone’s experience is a little different, but these answers cover what’s typical for most people.
Can My Postpartum Bleeding Stop and Start Again?
Yes, absolutely. It's incredibly common for postpartum bleeding to look like it’s tapering off, only to start up again. This little plot twist usually happens when you jump back into physical activity a bit too soon. Even a brisk walk or some light chores can be enough to trigger a temporary increase in flow.
For the most part, this isn't anything to worry about. But you should give your provider a call if the bleeding suddenly becomes heavy and bright red again after it had already lightened for a few days. The same goes for passing any large clots, that’s a sign to check in.
How Does Breastfeeding Affect Postpartum Bleeding?
Breastfeeding has a very direct effect on your bleeding. When you nurse, your body releases hormones that cause your uterus to contract. You might feel these as mild cramps or more intense "afterpains." These contractions often squeeze out a gush of blood either during or right after a feeding.
It might feel like you're bleeding more in that moment, but this is actually a good thing. This process helps your uterus shrink back to its pre-pregnancy size more efficiently, which can ultimately help the entire bleeding period end sooner.
What Is the Difference Between Lochia and My First Postpartum Period?
This is a great question, as it can be confusing! Lochia is the unique discharge that starts immediately after birth. Think of it as your body's way of cleaning house as your uterus sheds its lining and heals from where the placenta was attached. It follows a pretty predictable pattern, changing from red to pink to a yellowish-white over about four to six weeks.
Your first postpartum period, on the other hand, is your regular menstrual cycle making its grand return. This usually won’t happen for at least six to eight weeks after birth if you're not breastfeeding. If you are breastfeeding, your period could be delayed for many months. A period often starts with some spotting before building to a flow of fresh, red blood. The very end of lochia, in contrast, is typically a scant, whitish discharge. Knowing how long postpartum bleeding lasts is the best way to tell the two apart.
Finding the right support for your postpartum journey can make all the difference. At Bornbir, we connect you with vetted doulas, lactation consultants, and night nannies to help you feel confident and cared for. Find your perfect match in under 30 seconds.
