When you're expecting, the idea of labor can feel a little abstract, maybe even a bit intimidating. It helps to remember that labor isn't a single, sudden event. It's your body's natural process of giving birth, unfolding through a series of predictable stages that guide you from the first mild contractions all the way to delivering your baby and the placenta.
Your Roadmap for Understanding Labor and Delivery
Think of labor as a journey, not a sprint. Each part of this journey has its own unique purpose, physical sensations, and emotional landscape. Understanding this progression is powerful. It helps you know what's happening to your body, why it's happening, and how you can work with it every step of the way.
The entire process is generally broken down into three main stages, which act as signposts guiding you from the very first signs of labor until you're finally holding your newborn.
The Main Stages of Labor
Labor actually begins long before it's time to head to the hospital or birth center. It starts with an initial, often slow, phase and builds from there.
- Stage One: This is the longest stage, and it's divided into three distinct parts: early labor, active labor, and the transition phase. This whole stage is dedicated to your cervix opening (dilating) and thinning out to prepare for birth.
- Stage Two: This is the pushing stage. It officially begins when your cervix is fully dilated and ends with the incredible moment your baby is born.
- Stage Three: The final, and typically shortest, stage is the delivery of the placenta. This usually happens within 30 minutes of your baby's birth.
Knowing these key phases gives you a mental framework for what to expect. It helps you recognize where you are in the process and feel more prepared for what comes next.
Before we dive deeper, let's look at a quick overview.
The Stages of Labor at a Glance
This table offers a snapshot of what you can expect during each stage, from how your contractions might feel to your emotional state. Keep in mind that every labor is different, but this gives you a general idea of the progression.
| Labor Stage | Contraction Pattern | Cervical Dilation | What You Might Feel |
|---|---|---|---|
| Stage 1 (Early) | Mild, irregular, short (30-45 seconds) | 0 to 6 cm | Excited, anxious, "Is this it?" |
| Stage 1 (Active) | Stronger, longer, more regular (every 3-5 mins) | 6 to 8 cm | Focused, serious, need support |
| Stage 1 (Transition) | Intense, long, back-to-back (every 1-2 mins) | 8 to 10 cm | Overwhelmed, shaky, irritable |
| Stage 2 (Pushing) | Powerful, urge to push, may have a break between | 10 cm (fully dilated) | Focused, determined, exhausted but empowered |
| Stage 3 (Placenta) | Mild cramping as the uterus contracts | N/A | Relief, joy, focused on baby |
This roadmap can help you and your support team anticipate the shifts in your body and mind as you progress toward meeting your baby.
Labor is a uniquely personal experience, and no two births are exactly the same. Your journey will have its own rhythm and timeline. The goal is to feel informed and empowered, not to follow a strict set of rules.
This overview sets the stage for a deeper dive into each phase. As you prepare, remember that the care you receive throughout this time is essential. A great support system, from your partner to your medical team, makes all the difference. To better understand the comprehensive support available, you can learn more about what perinatal care is and how it covers this important period. With the right knowledge and team, you can approach your labor experience with more confidence and less anxiety.
The Three Stages of Labor Explained
Thinking about labor as one single, monumental event can feel pretty overwhelming. It's much easier to wrap your head around it if you see it as a process, a journey with a clear beginning, middle, and end. Labor unfolds in three distinct stages, and each one has its own purpose, rhythm, and set of experiences that bring you closer to meeting your baby.
Understanding these stages is like having a map for your journey. It helps you recognize where you are, anticipate what’s coming next, and, most importantly, work with your body’s incredible power instead of against it.
This visual timeline gives you a great overview of the typical progression, from those first mild contractions all the way to the arrival of your little one.
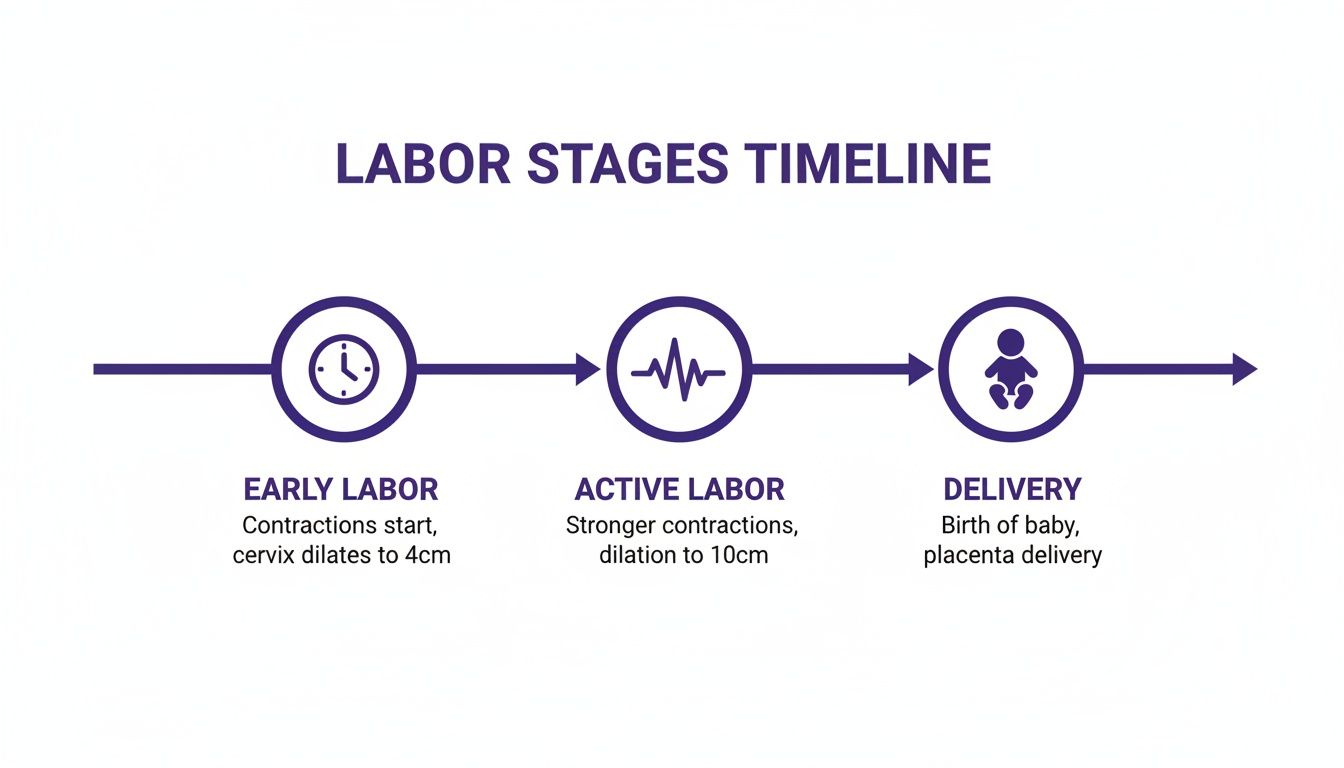
As you can see, the intensity and your focus shift dramatically as you move from the long, patient waiting game of early labor to the powerful work of active labor and finally, delivery.
Stage One, Part 1: Early Labor
Early labor is almost always the longest part of the entire process, but it's often the most manageable. Think of it as your body’s warm-up period. The main event here is your cervix starting to thin out (effacement) and open up (dilation) from 0 to about 6 centimeters.
Contractions during this phase are usually mild and might feel a lot like period cramps or a dull ache in your lower back. They tend to be irregular, coming anywhere from every 5 to 20 minutes and lasting for 30 to 45 seconds. Honestly, at this point, it can be tough to tell if you're experiencing real contractions or something else. If you're not sure, our guide on telling the difference between gas pains vs contractions can help clear things up.
Emotionally, you’ll probably feel a mix of excitement, nerves, and anticipation. This is the perfect time to rest, drink water, and save your energy. Most people spend this phase at home, walking around, watching a movie, or just trying to relax.
Stage One, Part 2: Active Labor
This is where the real work begins. Active labor is when your contractions become much stronger, more regular, and closer together. It's the unmistakable sign that your body is making serious progress.
During this phase, you can expect contractions to arrive every 3 to 5 minutes and last for about 60 seconds or even longer. They’ll demand your full attention, and you'll likely need to lean on your comfort measures, like breathing techniques or changing positions, to get through them. Your cervix will dilate from about 6 centimeters to 8 centimeters.
Active labor is when things get serious and your focus narrows. It’s often the point where you head to your hospital or birth center, as the intensity ramps up and you'll want more support from your birth team.
The length of active labor varies a lot from person to person. For first-time parents, the average active phase is around 7.5 hours, while for those who have given birth before, it’s closer to 3.3 hours. But it’s important to know that these are just averages. Long active labors are possible, with some first-time birthers experiencing a phase lasting up to 34.8 hours.
Stage One, Part 3: Transition
The final push of Stage One is called transition. It’s the shortest part of labor but by far the most intense. Your cervix is doing its final bit of work, opening from 8 to the full 10 centimeters needed for your baby to pass through.
Contractions during transition are powerful, long, and come one right after another, often every 1 to 3 minutes and lasting 60 to 90 seconds. You might feel an immense amount of pressure in your lower back and rectum. It’s also completely normal to experience physical sensations like shaking, chills, nausea, or even vomiting.
Emotionally, this is the most challenging part of labor. It’s common to feel overwhelmed, irritable, or even doubt your ability to keep going. This is the moment when the support of your partner, doula, and medical team is absolutely critical. Just remember, these intense feelings are a sign that you are so, so close to meeting your baby.
Once you hit 10 centimeters, the first stage of labor is officially complete. You’ve done the incredible work of opening the path for your baby, and now you’re ready to move into the second stage: pushing and delivery.
Finding Comfort and Managing Pain During Labor
Let's talk about one of the biggest topics on everyone's mind: pain. While pain is often a central part of the conversation around labor, it’s so important to remember you have a wide range of options for managing it. Every single birth is unique, and there is no "right" way to handle the physical sensations you'll experience.
The real goal is simply to find what works for you, moment by moment.
Empowering yourself with knowledge ahead of time helps you and your support team build a flexible toolkit. You might find yourself using several different strategies as your labor progresses, moving between non-medical and medical approaches as your needs change. That's completely normal.
Non-Medical Comfort Measures
Many people start off using non-medical techniques to manage contractions, especially in the early and active phases of labor. These methods are all about working with your body’s natural processes and can be incredibly effective. They often involve your partner or doula, making it a true team effort.
Some of the most common approaches include:
- Breathing Techniques. Never underestimate the power of your breath. Slow, deep breathing during contractions helps calm your nervous system, gets more oxygen to your muscles, and gives your mind something to focus on besides the intensity.
- Movement and Positioning. Staying active can make a world of difference. Walking, swaying, rocking on a birth ball, or getting on your hands and knees can help manage the sensations, use gravity to your advantage, and encourage your baby to move down.
- Massage and Counterpressure. Your partner or doula can provide amazing relief through touch. A simple back rub can be incredibly soothing, while firm, steady pressure on your lower back or hips during a contraction (known as counterpressure) can work wonders for intense back labor.
- Hydrotherapy. There's a reason so many people love laboring in water. Immersing yourself in a warm shower or a deep tub is a fantastic way to relax tense muscles and take the edge off the pain. The buoyancy provides a feeling of weightlessness and calm.
Labor is not just a physical event; it’s an emotional and psychological one, too. Creating a calming environment with dim lighting, soft music, and positive affirmations can help you stay centered and feel more in control of your experience.
These tools are there for you to use alone or in combination, giving you the flexibility to adapt as your labor shifts and changes.
Medical Pain Relief Options
As labor intensifies, you may decide you want or need medical pain relief. Knowing your options beforehand helps you make a clear-headed decision when the time comes. These interventions are safe and widely used, and choosing one doesn't diminish your birth experience in any way.
The most common medical options are designed to either reduce or completely eliminate the sensation of pain, allowing you to rest and conserve energy for pushing. They are always administered by an anesthesiologist or another trained medical professional.
Let’s break down the main choices.
- Epidural Block. This is the most common form of pain relief used during labor in the U.S. An epidural involves placing a tiny catheter in your lower back to deliver medication that numbs the lower half of your body, providing continuous relief.
- Spinal Block. Similar to an epidural, a spinal block is a single injection of medication into the spinal fluid. It works very quickly but for a shorter period, and it's often used for scheduled C-sections.
- Nitrous Oxide. You might know it as “laughing gas.” This is a mix of nitrous oxide and oxygen that you breathe in through a mask only during contractions. It doesn’t eliminate pain, but it can take the edge off and help you relax through the peak of the contraction.
Each option comes with its own set of benefits and potential side effects. For instance, an epidural provides excellent pain relief but may limit your mobility and can sometimes slow labor down. Nitrous oxide, on the other hand, is less invasive and wears off almost immediately, but it offers a much milder level of relief.
Making an informed choice is a personal decision. If you're weighing the pros and cons, you can learn more about the differences in our guide comparing nitrous oxide during labor vs an epidural. Ultimately, the best choice is the one that aligns with your birth preferences and helps you have a positive, empowered experience.
When to Go to the Hospital or Birth Center
Knowing the exact moment to grab your go-bag and head out the door is one of the biggest questions on every expecting parent's mind. It's a moment filled with so much anticipation, but having a few clear guidelines can help you feel way more confident when the time finally comes.
A great starting point, especially for first-time parents, is the 5-1-1 rule. This simple guideline suggests it’s time to call your provider and probably head in when your contractions are:
- Coming every 5 minutes
- Lasting for 1 full minute
- And have been following this pattern for at least 1 solid hour
This rule is a fantastic general guide because it usually means you're in active labor, not just the early warm-up phase. Arriving at the hospital too early can sometimes lead to interventions you might not have needed, so timing it right often helps things go a lot more smoothly.
More Than Just Contractions
While the 5-1-1 rule is super helpful, it’s not the only signal that it's "go time." Your body has other important ways of telling you what's up, and you should never ignore them. These are clear signs to call your doctor or midwife right away, no matter what your contractions are doing.
Keep an eye out for these key signs:
- Your Water Breaks. This might be a big gush of fluid like in the movies, but it could also be a slow, steady trickle you're not sure about. Even if you aren't having contractions yet, your provider needs to know.
- Significant Bleeding. A little bit of bloody mucus (what's called the "bloody show") is totally normal. But bright red bleeding, like a period, is not. Call your provider immediately.
- A Change in Baby's Movement. You know your baby’s daily rhythm better than anyone. If you notice they're moving a lot less than usual, don't wait. Get in touch with your care team.
- Intense Pain You Can’t Cope With. If your contractions feel completely overwhelming before they even get close to a 5-1-1 pattern, that’s okay. It's a perfectly valid reason to call for support and guidance.
Trusting your gut is a huge part of this process. If something just feels "off" or you have a powerful feeling that it's time to go, that is reason enough to check in. Your care team would much rather you call for a false alarm than have you wait at home feeling worried.
Understanding Labor Timelines
It's also helpful to know that labor timelines and even medical approaches can look different depending on where you are. For instance, in the United States in 2020, only 23% of births happened at or after 40 weeks of pregnancy. Compare that to the Netherlands, where that number was 44%. International data also shows that the average pregnancy length in the U.S. has shortened, going from about 39.1 weeks in 1990 down to 38.5 weeks in 2020. You can dig into the research on U.S. pregnancy lengths to learn more about these trends.
The most important takeaway here is to have an open, ongoing conversation with your provider. Make sure you talk about their specific guidelines for when to call and when to come in long before your due date arrives.
Ultimately, knowing when to go is about blending these guidelines with the unique signals your body is sending you. To get a better feel for what your body might be telling you, check out our guide on the signs that labor is near. Having this knowledge on your side empowers you to make the best call for you and your baby.
Building Your Birth and Support Team
Going through labor isn't something you have to do on your own. In fact, one of the most powerful things you can do to prepare is to build a solid, reliable support team. Having the right people in your corner can completely transform your birth experience, offering comfort, advocacy, and a steady hand when you need it most.
Your team can be anyone you trust, a partner, a dear friend, a family member, or professional support like a doula. The goal is simple: surround yourself with people who make you feel safe, heard, and truly empowered.
The Role of a Partner or Support Person
A partner or main support person is often the heart of the birth team. Their role is so much more than just being in the room. They can provide essential physical comfort, like applying that perfectly-placed counterpressure on your lower back during a contraction or just holding your hand with a reassuring squeeze.
Emotionally, their calm presence can be a huge anchor in the storm of labor. They can help you remember to breathe, whisper words of encouragement, and act as your advocate with the medical staff. To really shine in this role, it helps immensely if they understand your birth plan and feel ready to communicate your preferences clearly and kindly.
A well-prepared partner acts as your protector and your voice. They can manage the environment, field questions, and ensure your needs are being met so you can focus entirely on the work of labor.
Attending a childbirth class together or simply talking through your birth plan in detail can make all the difference, helping your partner feel confident and ready to be the best possible support on the big day.
Understanding the Doula Difference
While a partner offers that intimate, personal support, a doula brings professional expertise in comfort and advocacy. A doula is a trained professional who provides continuous physical, emotional, and informational support before, during, and right after childbirth. Think of them as a non-medical expert focused entirely on you and your well-being.
Their role is totally separate from that of a midwife or doctor. They don't deliver babies or perform clinical tasks. Instead, their job is to mother the mother. They offer:
- Physical Support: Suggesting new laboring positions when you feel stuck, providing massage, and guiding you through breathing techniques.
- Emotional Support: Offering constant encouragement, a calming presence, and unwavering reassurance when you start to doubt yourself.
- Informational Support: Helping you understand what's happening at each stage and translating medical jargon so you can make truly informed decisions.
The impact of having this kind of continuous support is well-documented. Studies consistently show that having a doula can lead to more positive birth outcomes, including a lower likelihood of certain medical interventions.
Finding the Right Professionals
Building your team is all about finding people you genuinely connect with. Whether you're choosing a midwife, an OB-GYN, or a doula, it’s critical to find professionals whose philosophy of care lines up with your own. You should feel completely at ease asking them questions and confident that they respect your wishes for your birth.
Platforms like Bornbir are designed to take the guesswork out of finding and vetting these essential support professionals, from doulas to lactation consultants. You can easily compare providers, read reviews from other parents, and connect with people who feel like the right fit for your family.
Learning more about what a birth doula does can also clarify if this type of support feels right for you. At the end of the day, your birth team is there to help you have the safest, most positive, and most empowering experience possible as you welcome your baby.
What Happens in the First Hour After Birth
The moment your baby arrives is absolutely breathtaking, but your body’s work isn’t quite finished just yet. This first hour, often called the "Golden Hour," is a profound time for bonding and recovery, along with a few final, gentle steps in the birth process. Knowing what’s coming can help you relax into this special window and feel more present.
Immediately after birth, your baby will likely be placed directly on your chest. This practice, known as skin-to-skin contact, is incredibly powerful. It helps regulate your baby’s temperature and breathing, calms them after the intensity of birth, and kicks off the release of hormones that support bonding and breastfeeding.
The Third Stage of Labor
While you’re soaking in those first precious moments with your newborn, your body is getting ready for the third and final stage of labor: delivering the placenta. This usually happens within 5 to 30 minutes after your baby is born. You might feel some mild cramping as your uterus contracts one last time to expel it.
Your doctor or midwife will carefully check the placenta to make sure it's all there. It's a standard and necessary step to ensure no fragments are left behind, which helps prevent complications.
Once the placenta is out, another important moment arrives.
Delayed cord clamping has become a standard recommendation, and for good reason. It just means waiting at least 30-60 seconds, or until the cord stops pulsating, before it's clamped and cut. This simple delay allows more iron-rich blood to transfer from the placenta to your baby, boosting their iron stores for months to come.
Routine Newborn Procedures
As you and your baby enjoy that close, skin-to-skin time, the nursing staff will perform a few gentle, routine checks. These are designed to be quick and minimally disruptive so you can focus on bonding.
These first assessments typically include:
- The Apgar Score. At one minute and five minutes after birth, your baby is given an Apgar score. This is a quick check-in on their heart rate, breathing, muscle tone, reflexes, and skin color. It's not a test they pass or fail, just a simple way to see how they’re transitioning to life on the outside.
- Vitamin K Shot. Newborns have low levels of vitamin K, which is essential for blood clotting. A small vitamin K injection is given to prevent a rare but serious bleeding disorder.
- Erythromycin Eye Ointment. A thin line of antibiotic ointment is applied to your baby’s eyes. This is a preventative measure to protect them from potential infections they might have been exposed to in the birth canal.
These procedures are all standard practice and are there to give your baby the healthiest possible start. Understanding what happens in this first hour helps you and your support team stay in the loop and advocate for your preferences, making sure those initial moments are as peaceful and positive as they can be.
Common Questions About Labor and Delivery
Even after you've read all the books and taken the classes, it’s completely normal to have a few “what if?” questions lingering in your mind. Let's walk through some of the most common ones that pop up as the big day gets closer.
A big one is always about food and drink. During early labor, feel free to have light snacks and drink plenty of water. You’ll need the energy. Once you hit active labor, though, your hospital's policy might change. Most providers suggest switching to clear liquids like broth or ice chips because your digestion slows way down.
And then there's the one everyone thinks about but is afraid to ask: pooping during pushing. It happens all the time! Seriously, it’s a good sign you’re using the exact right muscles to bring your baby down. Your birth team has seen it all before, they handle it discreetly, and it’s nothing at all to be embarrassed about.
What if My Water Breaks but I Have No Contractions?
This is a classic scenario that happens in about 8-10% of pregnancies. If you feel a gush or even a slow, steady trickle, the first thing to do is call your doctor or midwife. Don't wait. They’ll give you instructions based on your specific circumstances.
Usually, they'll ask you to come in to confirm that it's actually amniotic fluid. From there, you'll make a plan together. Sometimes, contractions will kick in on their own within 12 to 24 hours. If they don't, your provider will likely discuss inducing labor to minimize any risk of infection.
Your birth plan is a guide, not a contract. Labor can be unpredictable, so being open to changes and trusting your birth team is just as important as having a plan in the first place.
Can I Still Move Around with an Epidural?
Lots of people picture being stuck flat on their back once they get an epidural, but that’s not always the reality. While you won’t be up for a walk down the hall, modern "light" or "walking" epidurals can allow for more sensation and some movement in your legs.
With help from your partner or nurse, you can absolutely still shift positions in bed. Turning from side to side or using a peanut-shaped birthing ball between your knees can do wonders for helping labor progress, even with an epidural. It's a great question to ask your provider about ahead of time so you know what options your hospital offers.
Finding the right support for your pregnancy and birth journey makes all the difference. At Bornbir, we connect you with thousands of vetted doulas, midwives, and lactation consultants to build your perfect care team. Discover and compare local professionals to feel confident and supported every step of the way. Find your ideal birth support on Bornbir.
