When your breasts feel rock-hard and painful, the goal is a simple one: relief. Getting there involves a combination of frequent milk removal, some gentle massage, and using cold compresses to bring down that swelling. You're just trying to soften the breasts enough to feel comfortable and, more importantly, to help your baby latch on properly. This strategy helps manage your milk supply without accidentally telling your body to produce even more.
Understanding Why Breast Engorgement Happens
That sudden feeling of intense, painful fullness can be a real shock, especially for new parents. It typically pops up around day three to five postpartum, right when you feel like you're just starting to get the hang of things. This isn't just a simple sign that your milk has "come in." It's a bit more complex than that.
Engorgement is what happens during that natural shift from colostrum (your baby's first milk) to mature milk. Your body is ramping up milk production, but it's also dealing with a major increase in blood flow and other fluids rushing to your breast tissue.
Think of it like a traffic jam. You've got milk, blood, and lymphatic fluid all trying to get to the same place at once, causing a temporary backup of swelling and pressure.
The Real Impact of Fullness
This intense fullness can make your breasts feel hard as a rock, warm to the touch, and incredibly tender. Sometimes, the skin can even look shiny and stretched. For many, this is way more than just discomfort. It can actually make it difficult for your baby to get a deep latch, which is crucial for them to effectively remove milk.
The experience of engorgement is incredibly common, but that doesn't make it normal or something you just have to endure. Taking action quickly not only brings you relief but also protects your long-term breastfeeding goals.
Getting a handle on this phase is key. When milk isn't removed effectively, it can quickly escalate into more serious issues like clogged ducts or even mastitis, which is a painful breast infection. Our complete guide to Lactating 101 can offer more insights into navigating the early days of your breastfeeding journey.
A Common Postpartum Challenge
You are definitely not alone in this. Breast engorgement is so common among breastfeeding mothers that it's a primary reason some decide to stop breastfeeding earlier than they planned.
One study highlighted that the peak for engorgement happens on postpartum days three to five, with around 65% of mothers experiencing it severely enough to need help. By understanding what's happening in your body, you can take the right steps to manage the swelling and get back to comfortably feeding your baby.
When your breasts feel painfully full, your first thought is getting relief, and fast. The most effective strategy is actually pretty simple: frequent milk removal. The goal isn't to drain your breasts completely, which could accidentally signal your body to produce even more milk. Instead, it's all about getting just enough milk moving to ease the pressure.
The best way to do this is to feed your baby on demand, watching for their hunger cues. This responsive approach helps your body and your baby get in sync, regulating your supply to perfectly match what your little one needs.
If you're dealing with this, you are far from alone. The discomfort is incredibly common, with a staggering 69% of new mothers experiencing breast engorgement in those early postpartum days. It can turn what should be a joyful bonding time into a painful ordeal. The condition is usually a combination of milk, increased blood flow, and extra fluids hanging around in the breast tissue.
Making Latching Easier
One of the biggest frustrations with engorgement is that the breast can become so firm it’s tough for a baby to get a good, deep latch. When the areola is stretched taut, a baby might only manage a shallow latch, which isn't great for removing milk and can quickly lead to sore nipples.
A gentle technique called reverse pressure softening can make a world of difference here. Just before a feed, use your fingertips to apply steady, gentle pressure on the areola, right around the base of your nipple. Press inward toward your chest wall for about 60 seconds. This temporarily moves some of the fluid away, making the area much softer for your baby to latch onto.
You can also try a warm compress or a quick warm shower for a few minutes right before nursing. Heat encourages your let-down reflex, helping the milk flow more freely once your baby starts feeding. For more tips on making the whole experience more comfortable, check out our guide on how to stop breastfeeding pain.
Managing Swelling and Inflammation
After a feeding or pumping session, the focus shifts from encouraging milk flow to calming everything down. This is where cold therapy comes in. Applying a cold compress for 15-20 minutes can bring significant relief from that throbbing, swollen feeling.
Here are a few easy and effective options:
- Frozen Peas: A bag of frozen peas or corn wrapped in a thin towel is perfect because it can mold right to the shape of your breast.
- Chilled Cabbage Leaves: This is a classic home remedy for a reason. Chilled green cabbage leaves can be tucked right inside your bra. Many moms find them incredibly soothing, likely due to their shape, temperature, and natural anti-inflammatory properties. Just swap them out for fresh ones once they wilt.
- Gel Packs: Reusable cold gel packs designed specifically for breastfeeding are another great option to have ready in the freezer.
To make it even easier to remember what to do when, here's a quick summary of the go-to techniques.
Quick Relief Techniques for Engorgement
This table breaks down the core at-home remedies, clarifying when to use heat versus cold and the purpose of each action.
| Technique | When to Use | Why It Works |
|---|---|---|
| Warm Compress/Shower | Before feeding | Encourages the let-down reflex and helps milk flow more easily. |
| Reverse Pressure Softening | Before feeding, if areola is firm | Temporarily moves fluid away from the nipple, making it softer and easier for baby to latch. |
| Cold Compress/Cabbage Leaves | After feeding or pumping | Reduces swelling, calms inflammation, and soothes pain and discomfort. |
| Gentle Massage | During feeding or pumping | Helps move milk from congested areas toward the nipple. |
Using these methods in a cycle, warmth before, cold after, is a powerful combination for managing engorgement at home.
Beyond these direct relief methods, certain massage techniques can also help with the swelling. You can find helpful information in A complete guide to lymphatic drainage massage to learn about methods that support fluid movement. These immediate steps are all about gentle care, helping you manage the fullness without causing more irritation to already sensitive tissue.
Using Hand Expression and Pumping Strategically
When you’re dealing with the intense, rock-hard feeling of engorgement, your first instinct might be to grab a pump and drain your breasts completely. It seems logical, but it can actually backfire and make the problem worse.
The key is to think of hand expression and pumping as tools for relief, not for building up your milk supply. You only want to remove just enough milk to take the edge off the pressure and soften the breast. This small adjustment provides immediate comfort, makes it much easier for your baby to latch, and helps your body figure out exactly how much milk it needs to make without signaling it to produce even more.
The Gentle Art of Hand Expression
Hand expression is an amazing skill to have in your back pocket. It lets you release a small amount of milk without any equipment, which is perfect for softening the areola right before a feed when your breast is too firm for your baby to get a good latch.
Believe it or not, around 70.3% of mothers run into breastfeeding challenges like engorgement, and learning a simple technique like hand expression can be a game-changer. By gently squeezing to soften the areola, you can improve your baby's latch success by 40%, helping to clear the engorgement much faster than just pumping alone. You can read more about the research behind these breastfeeding challenges to see just how common this is.
Here's a quick guide to getting started:
- Position Your Hand: Make a "C" shape with your thumb and index finger, placing them about an inch or two behind your nipple.
- Press and Compress: Gently press your fingers straight back toward your chest, then squeeze them together.
- Roll and Repeat: Roll your fingers forward toward the nipple to express the milk. Find a steady rhythm and rotate your hand around the breast to drain from all sides.
Pumping for Relief, Not Removal
If you decide to use a pump, the same strategy applies. Steer clear of long, powerful pumping sessions that aim to empty the breast. That just sends a message to your body that your baby needs a ton of milk, which kicks off a frustrating cycle of oversupply and more engorgement.
Think of your pump as a pressure release valve. You're not trying to drain the tank, just let a little air out to make things more comfortable. This subtle shift in mindset makes a huge difference in managing engorgement.
Set your pump to a gentle setting and pump for just 5-10 minutes. Only when you feel you absolutely need to. This should be just enough to relieve that painful fullness without overstimulating your milk production. If you ever find yourself worried about not making enough milk, our guide on how to increase milk supply offers tips for the opposite scenario.
This simple visual breaks down the cycle for finding comfort. Start with warmth to get the milk flowing, then nurse or express just enough for relief, and finish with a cold compress to bring down the swelling.
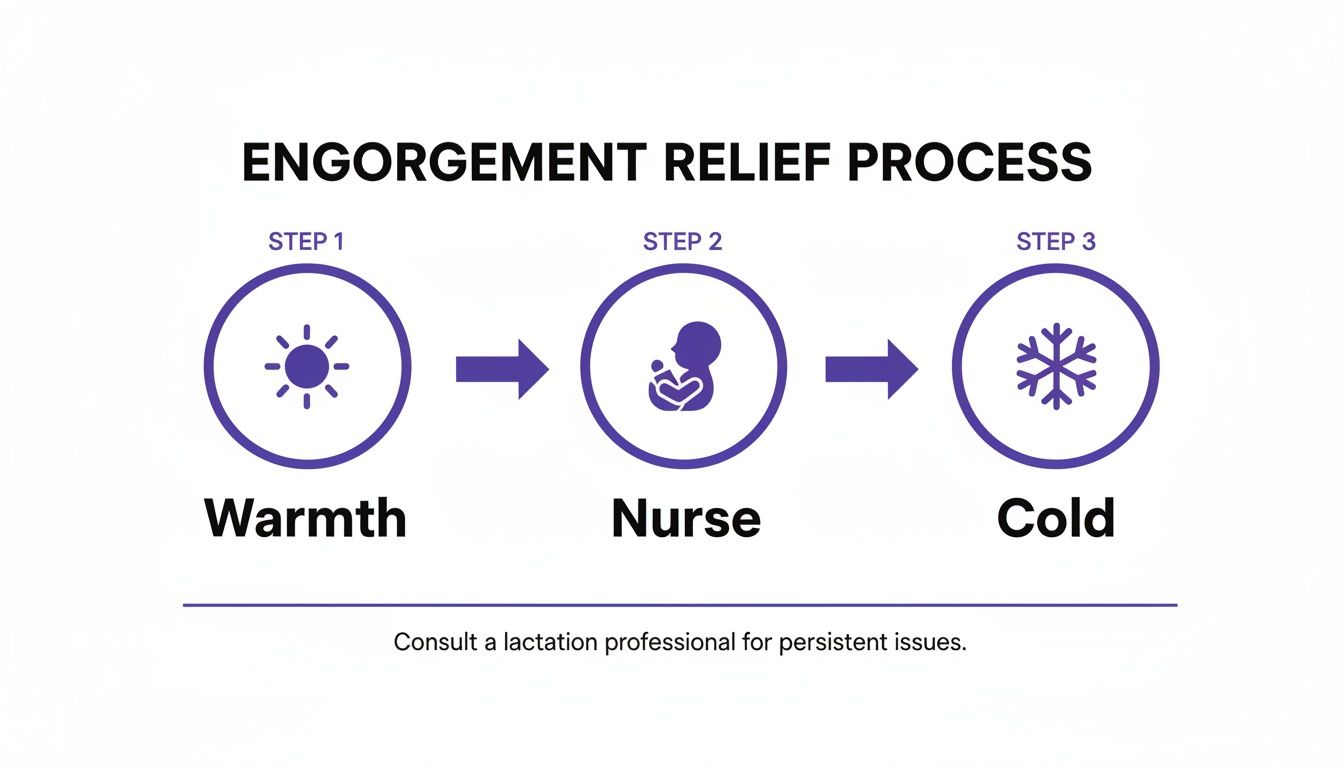
Following this warm-nurse-cold cycle consistently is a fantastic way to manage both the milk flow and the inflammation that comes with engorgement.
Proactive Tips to Prevent Engorgement
Managing engorgement is one thing, but avoiding it in the first place? Even better. By putting a few simple strategies into practice right from the start, you can make a world of difference in keeping your breasts comfortable and your milk flowing just right.
It all boils down to one core idea: respond to your baby’s needs to keep milk from backing up.
This process really begins right after birth. Nursing your baby as soon as you can, and then frequently after that, is the best way to establish a healthy milk supply and drainage pattern. This "early and often" approach helps sync your body's milk production with your baby's demand, which is the most effective way to head off that overwhelming, painful fullness.
Feed on Demand, Not by the Clock
Instead of watching the clock, watch your baby. You'll soon start to recognize their early hunger cues, like rooting (turning their head and opening their mouth), making little sucking motions, or bringing their hands to their mouth.
Feeding them when you see these signs, before they get really upset and start crying, is key. A calm baby is far more likely to get a deep, comfortable latch, which is absolutely essential for draining the breast effectively.
A deep latch is your best defense against engorgement. When a baby latches well, they effectively drain the breast, which prevents the painful backup of milk and fluid that leads to severe swelling.
A shallow latch, on the other hand, means less milk is removed and often leads to sore nipples. If you’re still expecting, getting a handle on the fundamentals now can set you up for success. You can learn more in our guide on how to prepare for breastfeeding.
Prioritize Latching Over Pacifiers Early On
In those first few weeks, it can be really helpful to hold off on introducing a pacifier. Every time your baby sucks at the breast, they're sending a direct signal to your body about how much milk to make.
Giving a pacifier too early can sometimes mask those important hunger cues, causing you to miss a feeding. When that happens, your breasts can quickly become overly full and uncomfortable.
Once your milk supply is well-established, usually around the 3-4 week mark, bringing a pacifier into the mix is much less likely to interfere. The goal is simply to let your baby’s needs exclusively drive your milk production during that critical initial period. By focusing on effective, on-demand nursing, you're teaching your body precisely what your baby needs, helping you sidestep the worst of the discomfort and find your rhythm together.
When To Call A Lactation Consultant Or Doctor
Most of the time, you can absolutely handle engorgement at home with the kinds of comfort measures and techniques we've talked about. But sometimes, you need to call in the professionals. Knowing when to make that call is so important for your own health and your baby's.
Always, always trust your instincts. If something just feels off, it’s better to reach out for help than to tough it out and wait. It's easy to feel overwhelmed, but severe pain that isn't getting better isn't just part of the deal. The right support can make a world of difference. To get a better handle on what a lactation consultant does, it's worth learning more about their role in situations just like this.
Signs Of A Possible Infection
One of the biggest worries with engorgement that just won't quit is that it can escalate into mastitis, which is a painful breast infection. This is something that needs medical attention, so you need to be able to spot the warning signs.
Call your doctor right away if you experience any of these symptoms, especially if they pop up suddenly:
- A fever of 100.4°F (38°C) or higher
- Flu-like symptoms, like body aches, chills, and just feeling wiped out
- A wedge-shaped red, swollen, or hot spot on your breast
- Red streaks appearing on your breast
- A burning pain that’s constant or happens when you nurse
These are the classic signs that simple inflammation has turned into a full-blown infection. Your doctor will likely prescribe antibiotics to knock it out. It's really important to keep nursing or pumping through it to keep the milk moving and help clear the infection.
When Your Baby Is Struggling
Engorgement isn't just about your own discomfort; it can make feeding incredibly difficult for your baby. When your breast is rock-hard and full, it can be nearly impossible for a little mouth to get a deep, effective latch. If this goes on for too long, it can seriously impact how much milk your baby is getting.
You are the expert on your baby. If you notice persistent feeding issues or signs that they aren't getting enough to eat, it’s time to call a lactation consultant or pediatrician.
Keep a close eye out for these red flags related to your baby's feeding and well-being:
- Consistently poor latch. You've tried reverse pressure softening and other tricks, but your baby just can't seem to latch on deeply.
- Signs of dehydration. This could look like fewer than six wet diapers in a 24-hour period (once your milk is fully in) or urine that's dark yellow.
- Significant weight loss or slow weight gain. Your pediatrician will be tracking this, of course, but if your baby seems lethargic or isn't gaining weight as they should be, that's a reason for an immediate call.
- Extreme fussiness or refusal to nurse. A baby who is constantly frustrated and popping off the breast might not be transferring milk well at all.
This is exactly where a lactation consultant shines. They can watch a feeding, assess your baby's latch, and create a plan tailored specifically for you. They're the experts in figuring out the mechanics of what's going on and can give you the hands-on support needed to get relief and feed your baby comfortably again.
Frequently Asked Questions About Engorgement
Navigating breastfeeding often feels like you're full of questions, and that's completely normal. When you're in the thick of engorgement discomfort, getting clear, straightforward answers can be a game-changer. Here are some of the most common concerns we hear from parents.
How Long Does Engorgement Typically Last?
For most new moms, that really intense, uncomfortable phase of engorgement hangs around for about 24 to 72 hours. I know it can feel like it will never end when you're in it, but this part is temporary.
If you stay on top of frequent milk removal, whether that’s your baby nursing or you're doing some strategic hand expression, you should start to feel a whole lot better within a couple of days. Your body is incredibly smart and will quickly start to regulate your milk supply to match what your baby actually needs.
Can I Take Pain Medication For Engorgement?
Yes, absolutely. Over-the-counter pain relievers that are generally considered safe for breastfeeding can make a world of difference in managing the pain and swelling.
Ibuprofen is often a great choice because it specifically targets inflammation, which is a huge part of what makes engorgement so miserable. Acetaminophen is another safe bet for just taking the edge off the pain. Of course, it's always a good idea to run it by your doctor or lactation consultant before starting any new medication, just to be sure it’s right for you.
Taking an anti-inflammatory can be a critical part of your comfort plan. It doesn't just dull the pain; it actively works to reduce the swelling that's causing all that pressure in the first place.
Many new mothers have questions about their milk supply. If you're looking to learn more, you can explore resources on topics like breast milk enhancers to better understand the different aspects of lactation. Arming yourself with knowledge can help you feel more confident as you move through your feeding journey.
Will Pumping Make My Engorgement Worse?
This is such a common and valid concern. The short answer is: it can, if you don't do it strategically. The classic mistake is pumping until the breast feels completely empty. This sends a powerful signal to your body to ramp up production, trapping you in a frustrating cycle of oversupply and even more engorgement.
The trick is to think of your pump as a tool for relief, not a tool for draining.
- Pump for Comfort Only: Just pump long enough to take the pressure off and soften the breast. This might only take 5-10 minutes.
- Keep Settings Gentle: Your breast tissue is sensitive right now, so high suction can be irritating. Start on a low setting and only increase it to a level that feels comfortable.
- Try Hand Expression First: Sometimes, all you need is to soften the areola enough for your baby to get a good latch. Hand expression is often a better, more gentle way to do this than hooking up the pump.
Your goal is to "take the edge off," not to "empty the tank." This approach gives you immediate relief without accidentally telling your body to make even more milk.
What’s The Difference Between Engorgement And A Clogged Duct?
It's so easy to mix these two up because they both involve breast pain, but they aren't the same thing. Knowing the difference is key to treating the problem correctly.
Engorgement usually affects the entire breast. You’ll likely feel that both breasts are hard, swollen, warm, and just generally achy. The feeling is widespread, not focused on one spot.
A clogged duct, on the other hand, is a more localized problem. It typically feels like a specific, tender lump or a firm, wedge-shaped area in just one breast. While severe engorgement can sometimes lead to clogged ducts if milk isn’t flowing freely, a clog itself is a specific blockage, not that all-over feeling of fullness.
At Bornbir, we know that having the right support makes all the difference. If you're struggling with engorgement or have other feeding questions, you can instantly connect with vetted, parent-reviewed lactation consultants in your area for in-person or virtual help. Find your perfect match and get the expert guidance you deserve by visiting https://www.bornbir.com.
