Deciding when and how to wean from breastfeeding is a deeply personal choice, one that looks different for every mother and baby. At its core, weaning is the process of gradually phasing out nursing sessions, giving both your body and your little one time to adjust to a new normal. It’s a major transition, closing one chapter of your feeding relationship and opening another.
Your Guide to Starting the Weaning Journey
There's no magic date on the calendar that signals the "right time" to start weaning. It’s a mix of your own readiness, your baby's developmental cues, and what works for your family's unique situation. The first real step is learning to recognize the signs that you or your baby might be ready for this emotional and physical shift.
The process can be parent-led, baby-led, or sometimes, it just happens naturally as a mutual decision over time. When you understand the cues, you can approach this change with more confidence and compassion for both of you.
Recognizing the Signs of Readiness
For your baby, readiness can show up in a few ways. You might notice they have a growing interest in solid foods, or maybe their nursing sessions have gotten much shorter. Some babies become easily distracted at the breast or start pulling away, showing less interest in nursing just for comfort.
For you, the signs might be more about logistics or your own feelings. You might be returning to work, feeling ready for more independence, or simply sensing that your breastfeeding journey has come to a natural end. There's no single "right" reason, only what feels right for you and your family.
Weaning is so much more than just stopping a feeding method. It's a huge developmental milestone for your baby and a significant emotional shift for you. It's okay to feel a mix of everything from relief to sadness, and acknowledging those feelings is a huge part of the process.
Many families around the world find themselves navigating this transition somewhere between the 6 and 12-month mark. Globally, only about 48% of infants under six months are exclusively breastfed. In the US, that number is much lower at 24.4%, dropping to 18.2% by six months, often due to things like returning to work or challenges with milk supply. These figures really highlight how common this transition is and why having good support is so critical.
Preparing for a Smooth Transition
Once you’ve made the decision, a little practical and emotional prep work can make all the difference. On the practical side, start thinking about what will replace those nursing sessions. Will you offer a bottle, a sippy cup, or a healthy snack? For those interested in fostering early independence, looking into a Montessori weaning table can offer some great ideas.
Emotionally, prepare yourself for a shift in how you connect. You can create new rituals to replace that special nursing time. Think extra cuddles, reading a book together, or singing a favorite song. The goal is to reassure your baby with your love and presence, showing them that your bond remains strong. For a deeper dive into the physical side of things, check out our guide on the fundamentals of https://www.bornbir.com/blog/lactating-101.
To help guide you, here are the core ideas to keep in mind as you get started. Think of these as your foundational principles for a gentle and respectful weaning process.
Key Weaning Principles at a Glance
| Principle | What It Means | Why It's Important |
|---|---|---|
| Gradual Reduction | Slowly decrease the number or length of nursing sessions over weeks, not days. | This allows your milk supply to decrease slowly, preventing engorgement and clogged ducts. It also gives your baby time to adjust emotionally. |
| Listen to Your Body | Pay attention to signs of discomfort like fullness or pain. Hand express for relief if needed. | Pushing too fast can lead to painful issues like mastitis. A gentle pace keeps you comfortable and safe. |
| Offer Comfort | Replace nursing with other forms of comfort, like cuddles, songs, or a favorite toy. | This reassures your baby that your love and connection remain strong, even as the feeding dynamic changes. |
Remember, these principles are flexible. The most important thing is to be patient with yourself and your baby as you navigate this new stage together.
Creating a Gentle Weaning Schedule That Works for You
Finding the right weaning schedule is less about a rigid calendar and more about tuning in to your body and your child's needs. There’s really no one-size-fits-all timeline. The whole idea is to make slow, gradual changes that give everyone a chance to adjust, both physically and emotionally.
Naturally, this process looks different depending on your little one's age and your family's rhythm. A plan that works beautifully for a six-month-old just starting on bottles will be miles away from the approach you'd take with a two-year-old who nurses mostly for comfort.
A good plan always starts with taking stock of where you are, getting ready for the shift, and then taking that first small step.
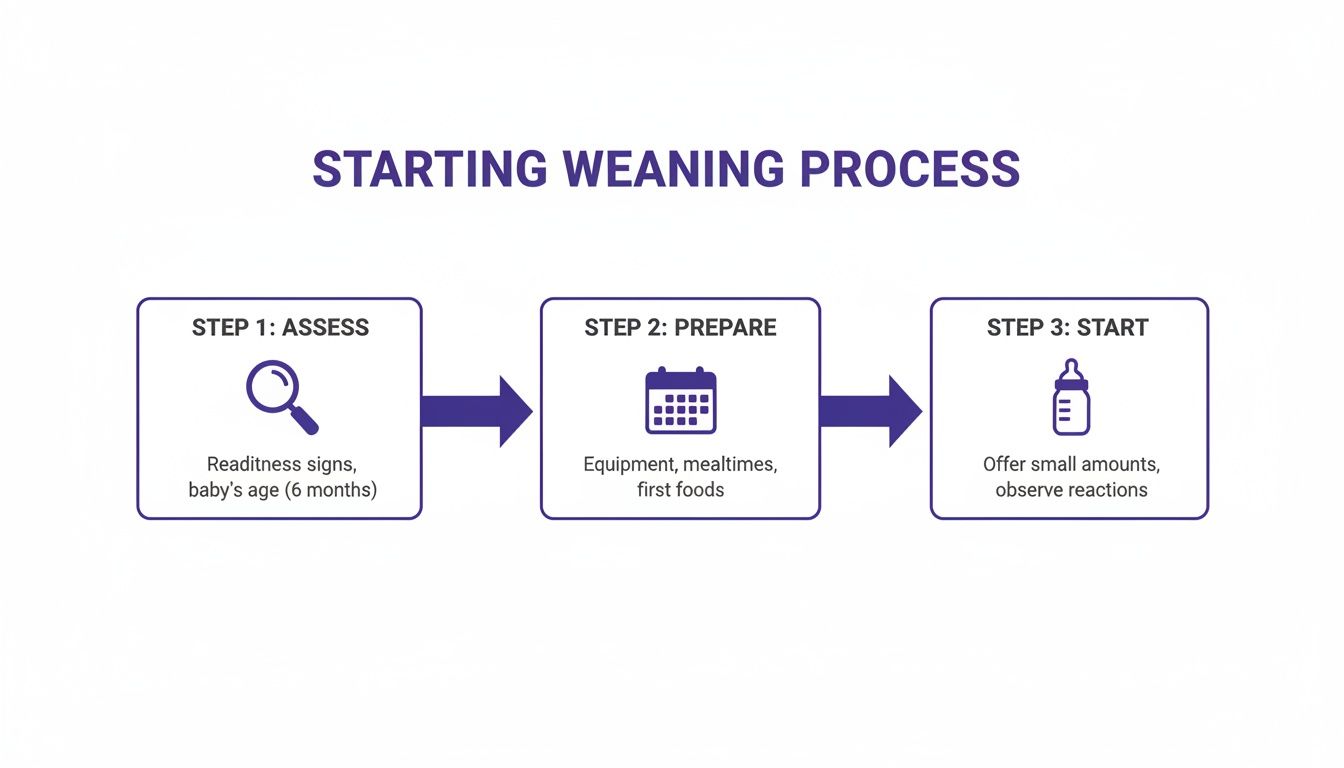
As you can see, the most successful weaning journeys begin long before you drop the first feed. It all starts with thoughtful planning.
Strategies for Babies Under One
For younger babies, the gentlest and most common path is dropping one feeding at a time. This simple strategy keeps you from getting painfully engorged and gives your baby time to get used to a bottle or sippy cup.
Begin by picking one nursing session to eliminate. Often, it's the one your baby seems least attached to. A mid-day feed is a great candidate because they’re more likely to be distracted by toys and playtime. Go ahead and replace that nursing session with a bottle of pumped milk or formula.
Wait at least 3-5 days before dropping another feed. This pause is so important. It lets your milk supply slowly decrease, which significantly lowers your risk of getting clogged ducts.
Don't rush it. If you're feeling overly full or you notice your baby is having a hard time, it's more than okay to slow down. Listening to your body and your baby is the most critical part of any weaning plan.
Once you both feel comfortable with the new routine, you can choose the next feeding to drop and do it all over again. The first-thing-in-the-morning and bedtime feeds are usually the last to go, as they tend to be the most comforting for babies.
Weaning Approaches for Toddlers
Weaning a toddler is often a completely different ballgame. They nurse for connection and comfort just as much as for nutrition, and their schedules can be all over the place. A strict plan probably won't fly here.
Here are a few strategies that work well for this age group:
- Don't Offer, Don't Refuse. This is a more passive but surprisingly effective method. You simply stop initiating nursing, but you don't say no if your toddler asks. By keeping them busy with fun activities, snacks, and drinks, you'll often find they start asking to nurse less on their own.
- Shorten Nursing Sessions. Instead of cutting a feed out completely, you can just make it shorter. Try saying, "We can nurse until I finish singing 'Twinkle, Twinkle, Little Star.'" Over time, the sessions get so brief that your toddler might just lose interest.
- Postpone and Distract. When your toddler asks to nurse, you can try saying, "Yes, we can do that soon! But first, let's finish this puzzle!" A lot of the time, the distraction works and they forget they even asked. This tactic is best for toddlers who can understand simple explanations.
Sample Schedules You Can Adapt
Sometimes, just seeing a schedule written out can make the whole process feel less overwhelming. Just remember, these are starting points. You'll want to tweak them to fit your life.
For a 7-Month-Old Baby (Dropping a Mid-Day Feed):
| Time | Day 1-3 (Old Routine) | Day 4-7 (New Routine) |
|---|---|---|
| 7 AM | Breastfeed | Breastfeed |
| 10 AM | Breastfeed | Bottle/Sippy Cup |
| 1 PM | Breastfeed | Breastfeed |
| 4 PM | Breastfeed | Breastfeed |
| 7 PM | Breastfeed | Breastfeed |
For a 15-Month-Old Toddler (Using 'Shorten & Distract'):
| Situation | Old Routine | New Routine |
|---|---|---|
| Wake Up | Nurse for 15 minutes | Nurse for 5-10 minutes, then offer a snack. |
| After Nap | Nurse for comfort | Offer a cuddle and a story first, then a sippy cup. |
| Bedtime | Nurse to sleep | Nurse for a few minutes, then transition to rocking/singing. |
Keep in mind that weaning can sometimes throw a wrench in sleep patterns. As you change your feeding schedule, you might need to revisit your child's sleep routine, too. For some helpful timelines, check out this guide to a newborn sleep schedule by week, which has insights you can adapt as your child grows.
No matter which schedule you try, the goal is always a gentle transition that feels right for both of you.
Managing Your Body Through the Weaning Process
Weaning isn't just about your baby; it's a major physical shift for you, too. As you start cutting back on nursing sessions, your body needs time to get the message and slow down milk production. The goal here is to manage this transition as comfortably as possible, steering clear of common hurdles like painful engorgement and clogged ducts.
Listening to your body is probably the most important thing you can do right now. When you drop a feed, it’s totally normal for your breasts to feel full or even uncomfortably firm for a day or two before they adjust. Your job is to manage that fullness without accidentally signaling your body to make more milk.
Preventing and Treating Engorgement
Engorgement is what happens when your breasts fill up with more milk than your baby is taking out. During weaning, it’s usually a sign that you might be dropping feeds a little too quickly for your body to keep up. The feeling can range from mild pressure to serious pain, so managing it the right way is key.
The number one rule is to avoid fully emptying your breasts. Pumping or nursing until empty will just tell your body to ramp up production again, the exact opposite of what you want. Instead, you can hand express or pump just enough milk to take the edge off. The goal isn't to be empty; it's just to be comfortable.
Here are a few other strategies that really work:
- Use Cold Compresses. A cold pack or even a bag of frozen peas wrapped in a cloth, applied for 15-20 minutes at a time, can work wonders for swelling and discomfort. The cold helps constrict blood vessels, which can help slow things down.
- Try Cabbage Leaves. This is an old-school remedy for a reason. Chilled, clean cabbage leaves tucked right into your bra can be surprisingly soothing and effective at reducing swelling. The enzymes in the cabbage are thought to help decrease milk supply.
- Wear a Supportive Bra. A good, supportive bra that isn't too tight can make a world of difference. Just try to avoid underwires or anything that digs in, as that can sometimes lead to plugged ducts.
For a deeper dive, you can find more detailed techniques in this helpful guide on https://www.bornbir.com/blog/how-to-relieve-engorgement.
Spotting Clogged Ducts and Mastitis
While engorgement is pretty common, you need to be on the lookout for more serious issues. A clogged or plugged duct will feel like a hard, tender lump in your breast that doesn't soften after a feed. The spot might also look red and feel warm.
If a clogged duct doesn't clear up, it can sometimes turn into mastitis, which is an inflammation or infection of the breast tissue.
Recognizing the signs of mastitis early is incredibly important. In addition to the breast pain and redness of a clogged duct, you might experience flu-like symptoms. Think fever, chills, and body aches.
If you think you have a clogged duct, it's important to continue nursing or expressing from that side to help clear the blockage. Gently massaging toward the nipple during a warm shower can also help. Just be careful not to be too aggressive, as new guidance suggests vigorous massage can actually increase inflammation.
When to Seek Medical Advice
You can often handle mild engorgement and some clogged ducts at home. But there are definitely times when you need to call your doctor or a lactation consultant for backup.
Reach out to a professional if:
- A clogged duct isn't getting better after 24-48 hours.
- You develop a fever or start feeling sick, which are tell-tale signs of mastitis.
- Any redness on your breast starts to spread or appears in streaks.
- You're in a lot of pain, and nothing you're doing at home is helping.
Mastitis usually requires antibiotics, so getting medical attention quickly is the best way to keep it from getting worse. Your well-being is a huge part of a successful weaning journey. As you navigate these changes, getting enough rest is crucial for your own recovery and well-being; you can find practical tips to help improve sleep quality during this period. Remember, taking care of yourself is just as important as taking care of your baby.
Navigating the Emotional Shift for You and Your Baby
Weaning is so much more than just a physical process. It’s a huge emotional milestone for both you and your child, and it's totally normal to feel a whole mix of things. You may feel pride, relief, sadness, or even a little guilt.
This transition marks the end of a really special connection, and it’s okay to sit with whatever feelings come up.
For your little one, nursing was never just about food. It was their go-to source for comfort, security, and closeness. As you figure out how to wean from breastfeeding, remember you’re not taking away your love; you’re just finding new ways to show it. The key is to be incredibly gentle with yourself and your baby as you both adjust.
Acknowledging Your Own Feelings
It can be surprising just how intense the feelings around weaning are. You might feel a real sense of loss for those quiet, cuddly moments you shared. These feelings can hit even harder if weaning happened sooner than you planned or for reasons you couldn't control.
On the flip side, you might feel a huge wave of relief and freedom. Getting some bodily autonomy back is a big deal, and it's perfectly fine to be excited about that. Many parents feel both sadness and relief at the same time, which can be pretty confusing. Just know that this emotional tangle is a completely normal part of the experience.
It’s also important to be aware of the hormonal rollercoaster happening in your body. The drop in oxytocin and prolactin, the hormones tied to milk production and bonding, can sometimes trigger mood swings or feelings of sadness.
Hormonal shifts during weaning are real and can absolutely impact your mood. If you feel overwhelmed by sadness or are struggling to cope, please talk to someone. A support group, a therapist, or your doctor can give you the help you need.
If your emotions feel particularly intense, it's a good idea to learn about the postpartum depression warning signs, as the risk for mood disorders can continue throughout the first year.
Supporting Your Baby Through the Transition
Your baby or toddler will have their own big feelings about weaning, too. They might be confused, frustrated, or just plain sad that their favorite source of comfort is changing. The best thing you can do is shower them with love and find new ways to connect.
The goal is to replace the comfort of nursing with other forms of affection and attention. This reassures them that your bond is as strong as ever, even if how you connect is changing.
- Offer Extra Cuddles. Physical touch is everything. Spend extra time snuggling on the couch, giving spontaneous hugs, or just holding them close throughout the day.
- Create New Rituals. Start a new special activity together. Maybe it's reading a book in your favorite chair, singing silly songs before a nap, or a gentle back rub at bedtime.
- Introduce a Comfort Object. For toddlers especially, a new stuffed animal or a special "cuddle blanket" can become a wonderful source of comfort when they can't nurse.
- Stay Present and Patient. If your child gets upset, validate their feelings. You can say something simple like, "I know you're sad we're not nursing now. I'm right here to cuddle you."
Strengthening Your Bond in New Ways
Try to think of weaning as a chance to discover new ways to be close. Your connection isn't ending; it's just evolving.
Every hug, every story, and every shared giggle builds on the beautiful bond you’ve already created. This transition calls for a lot of patience and compassion, for both of you. By focusing on that emotional connection, you can make weaning a positive experience that strengthens your relationship for years to come.
Practical Tips for Day, Night, and Naptime Weaning
Tackling daytime, naptime, and nighttime feeds can feel like you're managing three totally different projects. In many ways, you are. A mid-day nursing session might be about nutrition and a quick connection, while the feed right before sleep is deeply tied to comfort, security, and winding down.
The first step is recognizing the unique purpose behind each nursing session. A fun distraction that works wonders in the afternoon isn't going to cut it for a tired toddler seeking comfort in the middle of the night. You'll need a different approach for each scenario.

Strategies for Dropping Daytime Feeds
Daytime nursing sessions are often the easiest to drop first. This is usually because your child is more engaged with the world around them, making them way more open to alternatives. The key here is to be proactive.
Instead of waiting for your little one to ask to nurse, try to get ahead of it. Offer a fun snack or a sippy cup of water or milk before they even think about nursing. Timing this about 15-20 minutes before a usual feed can head off the request entirely.
This is also the perfect time to shake things up with new activities.
- Change Your Scenery. Do you always nurse in a specific chair after lunch? Try going for a walk or heading to the park at that time instead. Breaking the association with that spot can be surprisingly effective.
- Keep Busy. A new puzzle, a trip to the library, or a playdate can work wonders. A busy, engaged child is much less likely to think about nursing out of habit.
- Offer Quick Cuddles. Sometimes a quick hug is all they need to feel connected. Make sure they get plenty of physical affection that isn't tied to breastfeeding.
Creating New Nap and Bedtime Routines
Night and naptime feeds? That's a bigger challenge. These feeds are less about hunger and more about the powerful association between nursing and sleep. Weaning from them means creating a brand-new, comforting routine that signals it’s time to rest.
This process takes a lot of patience. Your goal is to gently separate nursing from the act of falling asleep. Start by nursing a little earlier in the bedtime routine, maybe before stories instead of right after.
A new bedtime routine is your most powerful tool for night weaning. The consistency of a bath, pajamas, stories, and songs creates a new sleep association that doesn't rely on nursing, giving your child a predictable and comforting path to sleep.
Once you’ve created that small buffer, you can start shortening the nursing session itself. Try nursing for just a few minutes, then unlatching your child while they are drowsy but still awake. Then you can rock, sing, or pat their back until they drift off. This is a critical step in teaching them how to fall asleep without you.
The Important Role Your Partner Can Play
Your partner can be your MVP, especially when it comes to night weaning. When a child wakes up looking for comfort, they often expect to nurse if they see or smell mom. Having your partner take over can break that deep-rooted expectation.
When the baby wakes up, your partner can be the one to go in and offer comfort. Rocking, soothing, or offering a sippy cup of water. The first few nights might be tough, but consistency is everything. Your child will gradually learn that waking up at night doesn’t automatically mean nursing.
This approach not only gives you a much-needed break but also helps your child learn to accept comfort from another loving caregiver. It’s a great way to reinforce that comfort comes in many forms.
To make it clearer, let’s break down which strategies work best for day versus night.
Day Weaning vs. Night Weaning Strategies
| Strategy | Best for Daytime | Best for Nighttime | Example |
|---|---|---|---|
| Distraction | ✅ | ❌ | When your toddler asks to nurse at 10 AM, you say, "Great idea! First, let's go see the squirrels outside!" |
| Substitute | ✅ | ❌ | Offer a tasty snack and a drink in a special cup about 20 minutes before a usual nursing session. |
| New Routines | ❌ | ✅ | Create a predictable bedtime sequence: bath, pajamas, story, song, cuddle, then bed. |
| Partner Support | ❌ | ✅ | When the baby wakes at 2 AM, your partner goes in to soothe them back to sleep instead of you. |
Ultimately, whether you're tackling day, nap, or nighttime weaning, the core principles are the same. Be patient, stay consistent, and shower your little one with love and reassurance as you both move through this big transition.
When to Get Professional Weaning Support
Let’s be honest: sometimes, even with the best plan, the weaning process hits a wall. This is completely normal. Knowing when to call in a professional is a sign of strength, and it’s often the best move for both you and your baby.
You don’t have to tough it out alone. Certified experts are there to offer personalized guidance when things feel overwhelming or you run into a problem you just can’t solve on your own. Their job is to make this transition smoother and far less stressful.
Recognizing When You Need an Expert
Many weaning bumps in the road can be handled with a little time and patience, but some situations really benefit from a professional’s touch. Think of it as calling in a specialist, just like you would for any other health concern.
It’s probably time to get help if you're dealing with persistent physical or emotional issues that just aren't improving. Constant discomfort or significant distress can take a real toll.
Consider reaching out if any of this sounds familiar:
- Recurring Clogged Ducts or Mastitis. If you keep getting painful clogged ducts or have had more than one bout of mastitis, something isn't right. An expert can help you uncover the root cause and map out a safer weaning plan to protect your health.
- Significant Emotional Distress. Feeling a little sad is one thing, but if you're battling overwhelming feelings of depression, anxiety, or grief tied to weaning, please talk to someone. The hormonal shifts during this time are intense and can seriously impact your mood.
- Persistent Breast Refusal from Your Baby. If your baby is under one and is consistently refusing a bottle or sippy cup to the point where you're worried about their hydration or nutrition, an expert can offer fresh strategies you haven't tried.
- Extreme Fussiness or Distress in Your Child. A little protest is normal. But if your baby or toddler seems inconsolable, is having major sleep disruptions, or is showing other signs of serious distress for a long time, professional guidance can help you find a gentler path forward.
Seeking professional support isn't a sign of failure. It's about getting the right tools for the job. A lactation consultant can provide a customized roadmap that respects your body, your baby's needs, and your emotional well-being.
Getting this specialized help can turn a stressful, confusing situation into a manageable one, giving you the confidence to move forward.
Who to Contact for Weaning Support
You have a couple of fantastic options when you need professional help with weaning. Who you call really depends on the specific problem you're facing.
For most weaning-related challenges, your first call should be to an International Board Certified Lactation Consultant (IBCLC). These professionals are the gold standard in lactation care, with extensive training in all things breastfeeding, including the complexities of weaning. If you want to better understand their role, our guide on what a lactation consultant does offers a great overview.
An IBCLC can help create a personalized, gradual weaning schedule that minimizes your risk of engorgement and clogged ducts. They are also brilliant at providing strategies for helping your baby accept a bottle and offering emotional support for both of you through the transition.
Your doctor or OB-GYN is your go-to for medical issues. You should contact them immediately if you suspect you have mastitis, as you'll likely need antibiotics. They are also the right resource if you are struggling with symptoms of depression or anxiety. Don’t ever hesitate to discuss your mental health with your doctor; they can connect you with the resources you need to feel better.
Weaning is a major life transition, and it’s more than okay to need a little extra support to get through it. Reaching out is a positive step toward a healthy and happy conclusion to your breastfeeding journey.
At Bornbir, we connect you with thousands of vetted lactation consultants, doulas, and postpartum support professionals who can provide the expert guidance you need. Find the right support for your family today at https://www.bornbir.com.
