Here’s a quick side-by-side of pain relief, mobility, and intervention odds for natural labor vs epidural. It boils down to how much feeling you want, how much moving matters, and what medical steps you’re fine with.
Quick Answer On Natural Birth Vs Epidural
Key Differences Between Natural Birth And Epidural
| Criteria | Natural Birth | Epidural |
|---|---|---|
| Pain Relief Method | Breathing techniques, position changes, massage | Local anesthetic injected near spinal nerves |
| Mobility Impact | Full freedom to walk, squat, and switch positions | Generally bed-bound with limited repositioning |
| Intervention Likelihood | Lower probability of forceps or vacuum | Slightly higher odds of assisted delivery |
This table lays out the basics to help you decide.
At A Glance
Key Insight Balancing full sensation against reliable pain control is at the heart of this choice.
- Pain Tolerance
Natural birth lets you ride every contraction, using breath, movement, and massage as your toolkit, an epidural quiets lower-body pain almost completely. - Mobility Goals
With no medication, you can change positions, walk the room, or lean on a birthing ball whenever you like, an epidural typically means staying in bed, with IV lines and monitors in place. - Intervention Likelihood
Studies link epidurals to a modest rise in forceps or vacuum-assisted deliveries, going unmedicated usually translates to fewer assisted-birth interventions. - Birth Plan Fit
Opt for natural if you’re aiming for minimal medical involvement, choose an epidural if you want predictable, targeted relief. - Backup Options
Keep nitrous oxide, counter-pressure techniques, or repositioning on your radar in case you switch paths mid-labor.
Who Benefits Most
- Birthers aiming for a low-intervention experience and full bodily awareness
- Those facing potential complications or lengthy labor who need dependable pain relief
- Anyone planning a hybrid approach, starting unmedicated then adding an epidural if comfort levels shift
You might find our guide on preparing for labor useful as you refine your plan.
Next Steps
Use these insights to shape questions for your care team, doula, or anesthesiologist:
- What’s the optimal time window for epidural placement to avoid slowing labor?
- How will pain relief timing sync with each stage of labor?
- Which mobility aids or positions should be ready, with or without medication?
Every birth setting is unique, so adapt these pointers to fit yours.
Understanding Natural Birth And Epidural
Looking at natural birth vs an epidural shows how each approach handles pain and movement in labor.
Natural birth uses breathing, gentle position shifts, and usually warm water to ease contractions.
Your body’s own oxytocin and endorphins then guide the baby’s descent.
How Natural Birth Works
In unmedicated labor, contractions build and fade, like waves you learn to ride.
Most birthing people explore different positions, like squats, hands-and-knees or gentle sways, to help the baby move down.
- Breathing Techniques: Deep inhales and steady exhales to match contraction rhythms
- Movement Strategies: Walking, swaying, or rocking to shift pain patterns
- Water Immersion: Warm baths or tubs to soften each surge and release tension
- Counterpressure: Firm support on the lower back during intense contractions
Natural birth gets you actively involved, tuning into feelings and adjusting as you go.
You can pivot positions instantly when a contraction pattern shifts, listening closely to your body.
- Immediate sensory feedback helps you fine-tune comfort in real time
- No medication side effects often means quicker postpartum recovery
For instance, Sara discovered that kneeling on hands-and-knees eased her back labor pain almost immediately, turning a tense moment into manageable comfort.
How Epidural Analgesia Works
An epidural involves placing a tiny catheter near your spinal nerves to block pain signals below the waist.
This targeted approach delivers consistent relief, allowing you to rest between contractions.
- Needle Placement: Performed by an anesthesiologist under sterile conditions
- Continuous Infusion: A slow drip of anesthetic to maintain numbness, adjustable as needed
- Monitored Mobility: Typically requires bed rest, though you can still shift laterally
Limited mobility means you’ll need support for repositioning, bathroom breaks, and posture changes, some people notice drops in blood pressure, headaches, or lingering numbness after delivery.
An epidural offers reliable pain control but often turns labor into a more medicalized process.
A 2008 CDC survey revealed that 61% of birthing people chose epidural or spinal anesthesia, while 39% delivered without medication. Learn more about these medicated birth statistics
It shows how epidurals have become the most common pain-management choice in U.S. hospitals.
Deciding between natural birth and an epidural often comes down to your comfort goals and how much mobility you want.
Explore how different providers support each birth approach with our guide on midwife roles versus obstetrician care: Difference Between Midwife and Obstetrician
Comparing Pain Relief And Labor Progress
Choosing between unmedicated birth and an epidural isn’t just about pain…it’s about timing and momentum too. We’ll explore research and real stories to illustrate how each path shapes your labor journey. By the end, you’ll know what to expect and how to talk it through with your care team.
Self-Reported Pain Levels
Many birthing people describe natural contractions as sharp peaks they ride with breathing, movement, and focused techniques, an epidural often brings pain scores down from 8 out of 10 to around 2 or 3 on a visual scale.
- Natural Birth Coping
• Rhythmic breathing and shifting positions
• Massage, counterpressure, or hydrotherapy - Epidural Relief
• Steady, even analgesia through labor
• Opportunity to rest during intense contractions
Some compare unmedicated labor to “turbulent waves you learn to surf,” others say an epidural can feel like “gentle pressure, not pain.”
Duration Of Labor Phases
Switching pain relief methods can nudge your labor clock. Below is a side-by-side look at median durations:
| Phase | Natural Birth (Median) | Epidural (Median) |
|---|---|---|
| First Stage | 6 hours | 7.5 hours |
| Second Stage | 60 minutes | 80 minutes |
| Total Labor | 7 hours | 9 hours |
A slight stretch in active and pushing phases with an epidural often ties back to reduced leg mobility and hormonal shifts, still both timelines stay within common ranges.
Assisted Delivery Rates
Epidurals can increase the odds of forceps or vacuum use, reflecting how pain relief intersects with intervention thresholds. Cochrane reviews report a 44% higher relative risk of assisted vaginal birth when an epidural is involved.
Key Insight
The likelihood of forceps or vacuum rises by nearly half with an epidural.
| Intervention | Natural Birth Rate | Epidural Rate |
|---|---|---|
| Forceps/Vacuum | 10% | 14.4% |
Read more about epidural intervention risk in this study: Read the full research about epidural intervention risk
Hormonal And Mobility Effects
Every contraction in natural labor pulses with oxytocin and endorphins, fueling progress and pain tolerance, when an epidural enters the picture, oxytocin surges can soften, and those instinctive urge-to-push sensations may linger.
- Oxytocin Release: Peaks in sync with contractions
- Endorphin Production: Heightens natural coping
- Mobility Impact: Limited position changes can slow descent
Expert Tip
Keeping your body moving, walking, swaying or rocking, can boost hormone flow and potentially shorten active labor.
When To Expect Shifts In Flow
Labor doesn’t stay the same for long. Here’s how pain relief might match each phase:
- Early Labor (0–4 cm)
Often manageable with movement and breathing. - Active Labor (4–7 cm)
Contractions speed up, many opt for stronger relief here. - Transition (7–10 cm)
The most intense phase, careful positioning and pain control can make a big difference.
Combining Techniques For Hybrid Approaches
If you want pain control and some freedom to move, consider a phased plan:
- Start with water immersion or upright work in early labor
- Introduce nitrous oxide for moderate contractions
- Move to a low-dose epidural once you hit active labor
This sequence preserves mobility early on and ensures comfort when things ramp up.
Real-World Case Vignettes
Two stories highlight how timing shapes each labor:
Case A: Natural Birth
- Anna shifted between squats, lunges, and walking
- First stage: 5.5 hours | Second stage: 50 minutes
- No forceps or vacuum
Case B: Epidural
- Beth chose a low-dose epidural at 5 cm
- First stage: 8 hours | Second stage: 90 minutes
- Delivered safely with vacuum assistance
These examples show how choices around pain relief, positioning, and intervention can connect to different labor rhythms.
Practical Tips For Shifting Labor Flow
Whether you plan to go unmedicated or request an epidural, these strategies can support both comfort and progress:
- Low-Dose Epidural Options
Ask about formulations that let you feel and move more. - Position Changes
Try hands-and-knees, side-lying, or standing to help dilation. - Massage & Hydrotherapy
Tools like a peanut ball or warm shower can ease transitions. - Nitrous Oxide As A Bridge
A mild inhaled choice ideal for early labor support.
For a deeper dive into inhaled options and epidurals, visit our guide: Nitrous Oxide During Labor Vs Epidural Guide
By blending approaches or adjusting timing, you’ll find a rhythm that balances pain relief with efficient progress. Use these insights as a springboard when you talk through your ideals and limits with your care provider.
Weighing Risks Benefits And Mobility Impact
Deciding between a natural, unmedicated birth and an epidural often comes down to how much freedom of movement you want versus the medical safeguards you need. Active positioning can jump-start labor, while an epidural offers consistent pain relief and close clinical monitoring.
A landmark Scottish study of over 500,000 births reported a 35% reduction in severe maternal morbidity when an epidural was used. Learn more in this deep dive at Evidence Based Birth.
- 35% Drop in Severe Complications. Epidural analgesia eases anxiety for those with medical concerns.
- Quicker Recovery & Skin-to-Skin. Unmedicated labors often lead to faster postpartum mobility.
- Vitals Monitoring. Teams track blood pressure and fever, intervening swiftly with fluids or meds.
Safety And Trade Off Scenarios
In higher-risk pregnancies, think preeclampsia or clotting disorders, an epidural’s protective effect often outweighs any mobility trade-off. Providers may recommend it to stabilize blood pressure and reduce hemorrhage risk.
Low-risk folks, however, frequently find that riding natural oxytocin surges and changing positions can shorten labor without medication.
- Preeclampsia or bleeding risks usually prompt an epidural recommendation
- Healthy lab results and no underlying conditions make unmedicated choices viable
- Severe asthma or cardiac issues sometimes steer the decision toward epidural support
Mobility And Labor Flow
Moving freely can cut active labor by up to 20%, thanks to stronger contractions in upright positions. Conversely, epidurals tend to extend the first and second stages by about 1–2 hours since leg sensation is reduced.
- Ask about mobile epidural catheters to walk or lean safely
- Use a peanut ball between your knees to open the pelvis in bed
- Request intermittent monitoring so you can shift positions without interruption
Postpartum Recovery And Breastfeeding Connection
Getting on your feet soon after birth helps restore bladder and bowel function and cuts blood-clot risks. While epidurals may delay your first urge to push or initial milk transfer, they often lead to calmer, more focused feeding sessions.
Read also: Pelvic Floor Exercises During Pregnancy to strengthen your muscles before labor.
- Early ambulation lowers deep vein thrombosis risk
- Controlled pain relief allows you to tune into newborn cues and latch techniques
- Regaining leg feeling supports positioning baby for nursing
Key Insight
When mobility meets reliable pain control, many parents report smoother recoveries and stronger feeding starts.
Hormonal Effects And Pelvic Mechanics
Natural labor primes oxytocin release, boosting contraction strength and deepening parent-baby bonding. Plus, endorphins flood your system when you move freely, easing discomfort naturally.
Epidurals may blunt some hormone surges but prevent cortisol spikes that come with unmanaged pain.
- Oxytocin peaks when you change positions and stay upright
- Endorphin production soothes you through each contraction wave
- Lower cortisol after an epidural can calm stress responses for both parent and baby
Rare Effects Versus Comfort Gains
Skipping medication avoids any drug-related side effects but usually means seeking extra support for intense surges. Epidurals carry minor risks postdural headaches or low-grade fevers in about 2% of cases, but most complications are managed quickly and effectively.
| Side Effect | Natural Birth | Epidural |
|---|---|---|
| Postdural Headache | N/A | 0.5% incidence |
| Fever After Delivery | Rare | 2% incidence |
| Allergic Reaction | Very rare | Extremely rare |
Your ideal mix of mobility and pain relief will shape how satisfied you feel about the whole experience. Use these details to guide your birth plan discussion.
Long Term Satisfaction And Recovery
Long-term happiness often hinges on whether your birth unfolds the way you imagined, whether that included intense, natural contractions or precise, low-stress pain control.
- Natural labor can mean quicker walking and less pelvic discomfort at two weeks postpartum
- Epidural users often cherish the moment they felt pain-free for the first time in labor and remember how calm contractions became
Ultimately, weighing risks, benefits, and movement needs helps you craft a birth experience that feels right for you.
When To Choose Natural Birth Or Epidural
Deciding between a natural (unmedicated) birth and an epidural comes down to your medical profile and personal priorities. If you prize mobility and want to follow your body’s rhythm, natural methods may serve you well. On the other hand, if steady pain relief and blood pressure control top your list, an epidural can be a solid choice.
Below, we dive into scenarios where one approach often outshines the other, helping you shape a birth plan that feels right for you.
Low Risk Birth Scenarios
When you enter labor with a healthy pregnancy and no complications, moving freely can make a world of difference. Simple shifts in position or a soothing soak can tap into your body’s natural pain-relievers.
- Upright Positions
Squatting or leaning on hands and knees uses gravity to your advantage, potentially shortening active labor by 20%. - Water Immersion
Laboring in a tub may lower stress hormones by around 40%, while giving you room to change postures easily. - Case Study A
Maria spent five hours alternating between a birthing tub and standing stretches. She never needed instruments or extra meds.
“Water gave me constant relief, and I felt in charge of my labor,” reflects a midwife with over a decade of hands-on practice.
These examples show how, when medical risk is low, staying upright and in motion can keep contractions efficient and pain manageable.
Medical And High Stress Scenarios
Certain conditions call for tighter control of pain and blood pressure. An epidural can calm severe hypertension and blunt stress-induced cortisol spikes in tense, prolonged labors.
- Epidural Indications
- Preeclampsia or high blood pressure risk
- Active labor lasting over 8 hours
- Twin gestation or breech presentation
- Low-Dose “Mobile” Epidurals
Some anesthesiologists offer lighter doses that still allow limited standing or side-lying adjustments.
| Scenario | Recommended Approach |
|---|---|
| Low risk, no complications | Natural birth |
| High risk or clear medical need | Epidural |
Studies suggest using an epidural in these situations can cut severe maternal or fetal complications by up to 35%.
Contraindications And Special Cases
Not everyone is a candidate for an epidural. If you have a low platelet count or a skin infection at the injection site, you’ll need to lean on other pain relief tools.
- Contraindications
• Platelet count below 100,000
• Skin infection on the back
• Severe spinal deformities - Alternative Techniques
• Nitrous Oxide for mild, quick-onset relief
• TENS Units to disrupt pain signaling
• Counterpressure, massage, and acupressure
These methods can fill the gap when an epidural isn’t an option, offering genuine comfort without medications.
First Time Versus Experienced Parents
Your birth history also plays a role. First-timers tend to have longer labors and often request an epidural around 4 to 5 cm dilation. Experienced parents might choose to stay unmedicated longer, knowing exactly how their bodies respond.
- First-Time Parent Tips
• Begin upright work and water immersion early
• Keep nitrous oxide on standby as a bridge
• Discuss a low-dose epidural for the transition phase - Multipara Strategies
• Rotate positions every 30–60 minutes in early labor
• Use a peanut ball if you do get an epidural
• Coordinate timing closely with your care provider
Key Takeaway: Mobility boosts oxytocin and can speed each phase of labor, while well-timed pain relief maintains forward momentum when complications arise.
Use these insights to fine-tune your birth plan and prepare questions for doulas, midwives, or anesthesiologists on Bornbir. Your comfort, safety, and joy matter most, so stay flexible, trust your instincts, and be ready to adapt as labor unfolds.
Creating Your Decision Checklist And Finding Providers
A personalized checklist cuts through the noise, spotlighting what matters most in your choice between a natural birth and an epidural. By the end, you’ll have targeted questions ready for your doula, midwife, or anesthesiologist.
The infographic below maps out a decision tree, showing how risk factors guide you toward a drug-free birth or an epidural.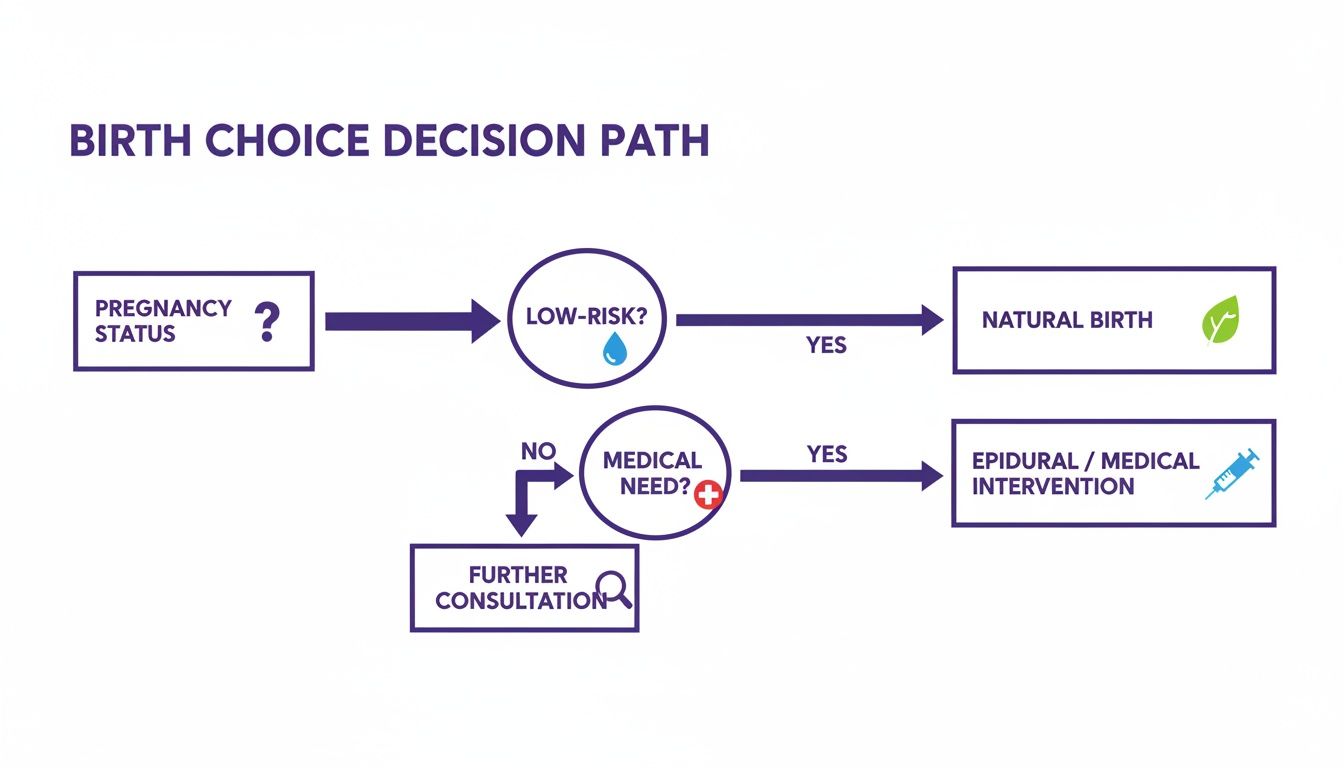
Notice how a low-risk profile leans toward unmedicated support, while clear medical needs point to epidural safety.
Clarify Your Core Preferences
Begin by jotting down what you value most during labor and delivery.
- Pain Management Priority – Weigh the benefits of breathing techniques and massage versus predictable relief
- Movement Freedom – Decide whether full mobility or partial bed rest fits your comfort
- Intervention Tolerance – Define your openness to forceps, vacuum or other tools
- Recovery Goals – Choose between faster postpartum mobility or a more controlled, calm experience
- Support Techniques – Pick from water immersion, counterpressure or an epidural, depending on your style
These bullet points become your north star when you compare provider offerings.
Build Your Question List
Now, turn preferences into probing questions that cover timing, dosage, and mobility.
- When is the optimal window to request an epidural without slowing labor?
- What dosage options allow me to maintain sensation and movement?
- How will I stay mobile if I want to walk or shift positions?
- Which natural techniques do you support, like water immersion or counterpressure?
- How do you coordinate with doulas or midwives during labor?
- What backup plan do you offer if one method falls short?
“Ask about movement options up front to avoid surprises when labor kicks in.”
– Sarah, Certified Doula
Learn more about building your birth plan in our guide on How to Create a Birth Plan.
Find Providers Who Fit Your Plan
On Bornbir, filter perinatal pros to match your checklist keywords—think natural birth support or epidural-friendly.
- Filter by credentials and years of experience for trust and safety
- Read real parent reviews to see how providers handle mobility and comfort
- Compare availability and pricing side by side to keep your budget on track
Real-World Example:
One parent found a midwife with 95% positive reviews for upright labor techniques. Another matched with an anesthesiologist specializing in low-dose, mobile epidurals just weeks before her due date.
“Your provider’s flexibility can make or break how you live out your birth plan.”
– Dr. Nguyen, Obstetrician
Rate And Compare Consultations
After each interview, use a simple scoring system to capture impressions and avoid second-guessing.
| Benchmark | Rating Scale |
|---|---|
| Communication Clarity | 1–5 |
| Empathy And Values | 1–5 |
| Flexibility | 1–5 |
Once you total your scores, the highest-ranking providers will stand out. Aim for 3–5 top picks before scheduling video calls.
Explore Community Feedback
Tap into Bornbir’s community threads for candid mom stories and quick case studies.
- Join local group chats for in-hospital and home birth experiences
- Note common praise points and red flags in reviews
- Browse provider profiles for photos, videos, and client quotes to gauge their vibe
This structured approach cuts through confusion in the natural birth vs epidural debate. You’ll feel confident moving forward with a team that truly aligns with your vision.
Frequently Asked Questions
How Long Can An Epidural Last?
Many expectant parents ask, “How long can an epidural catheter remain in place?” In practice, it stays safely for up to 24 hours, sometimes even longer with close monitoring.
Medical teams check blood pressure and sensory response every 2 hours, keeping your pain relief consistent through both active and pushing phases.
For example, Sarah relied on an epidural for 18 hours straight. Small dose tweaks kept her comfortable, but still able to shift and adjust on the bed.
What Nonmedicated Pain Relief Methods Have The Best Results?
If you’re exploring unmedicated options, research highlights a few clear winners:
| Method | Effect | Notes |
|---|---|---|
| Water Immersion | Lowers stress hormones by up to 40% | Warm water soothes tight muscles |
| Counterpressure & Massage | Eases contraction peaks | Targets lower back tension |
| Movement Techniques | Boosts oxytocin flow | Walking, squats, birthing ball shifts |
“Combining movement and massage can cut active labor by 20%,” notes a seasoned birth coach.
How Does Switching To An Epidural Mid-Labor Work?
Changing course mid-labor is surprisingly straightforward once you hit 4 cm dilation. Here’s how it unfolds:
- Confirm dilation of 4 cm or more,
- Sit or lie on your side for placement,
- Anesthesiologist threads the catheter and tests a small dose,
- Expect tingling within 10 minutes, with pain dropping from an 8 out of 10 to about 3 or 4 out of 10.
Influence Of Movement On Labor Speed
Remaining upright and changing positions can shave roughly 20% off active labor time.
Every step, side lunge, or gentle sway nudges your body to release more oxytocin and endorphins, nature’s labor accelerators.
Even after getting an epidural, you might still tilt your pelvis by lying on your side or by using a peanut ball.
Key Insight: Track your position every 30 minutes to discover which movements truly move labor forward.
Finding the right support shouldn't add to your stress. With Bornbir, you can easily search for lactation consultants, doulas, and other perinatal professionals who are familiar with the insurance landscape. The platform allows you to filter providers and connect with the right expert for your family, saving you time and giving you peace of mind. Find your perfect match at https://www.bornbir.com.
