Nipple thrush is a yeast infection, plain and simple. It’s caused by an overgrowth of Candida albicans, a type of fungus that lives on our skin all the time without causing any trouble. But when certain things throw your body’s natural balance out of whack, this yeast can multiply and turn into a painful infection on your nipples.
This often kicks off when there's an existing infection somewhere else, like oral thrush in your baby, which creates a frustrating cycle of passing the infection back and forth.
Understanding What Causes Nipple Thrush
Think of your skin as a bustling ecosystem, like a garden. It’s home to a healthy mix of good bacteria (the flowers) and naturally occurring fungi like Candida (the weeds). Usually, the flowers keep the weeds from taking over. But what happens when something comes along and disrupts this delicate balance?
That’s exactly what happens with nipple thrush. Certain triggers can knock back the good bacteria, giving the Candida weeds a golden opportunity to grow out of control. This isn't about being unclean. it's about a microbial imbalance. The warm, moist environment of a nursing parent's nipple area is the perfect breeding ground for this yeast once the balance is tipped.
The Parent and Baby Connection
One of the most common ways nipple thrush gets started is through the direct connection between you and your nursing baby. If your baby has oral thrush, the Candida fungus can easily transfer from their mouth to your nipples during a feeding session.
This can create a maddening "ping-pong" effect, where the infection is passed back and forth until both of you are treated at the same time. Since oral thrush is pretty common in babies, affecting about 24% of infants before they’re 18 months old, it’s a major risk factor for breastfeeding parents.
This back-and-forth cycle is precisely why treating just one person rarely works. The infection can linger, causing ongoing pain and discomfort that can seriously disrupt your breastfeeding journey.
Key Contributing Factors
Several other conditions can create the perfect storm for a Candida overgrowth. You can think of these as things that might weaken the "flowers" in your garden, letting the "weeds" run rampant.
Here's a quick look at the primary factors that can contribute to nipple thrush.
Key Factors Contributing to Nipple Thrush
| Contributing Factor | How It Increases Risk |
|---|---|
| Antibiotic Use | Antibiotics can wipe out the beneficial bacteria that normally keep yeast populations in check. |
| Nipple Damage | Cracks or sores from a poor latch create an easy entry point for the fungus to start an infection. |
| Weakened Immune System | Stress, exhaustion, or illness can lower your body's natural defenses against infections. |
| Excess Moisture | Damp breast pads or bras trap moisture against the skin, creating a warm, damp environment where yeast thrives. |
Understanding these risk factors is the first step toward both treating and preventing this incredibly uncomfortable condition.
A few key culprits stand out:
- Antibiotic Use: A recent round of antibiotics can be a major trigger, as it often eliminates the good bacteria that keep yeast under control.
- Nipple Damage: Cracked, sore, or damaged nipples from a less-than-perfect latch provide an open door for the fungus to get in and set up shop.
- Weakened Immune System: Being run-down from stress, lack of sleep, or illness can lower your body's ability to fight off infections, including yeast.
- Moisture: Leaving damp breast pads or bras against your skin for too long creates that warm, moist environment Candida just loves.
Getting a handle on these factors is crucial for getting relief and preventing future flare-ups. For more tips on establishing a comfortable nursing routine, check out our guide on lactating 101.
The Hidden Triggers Behind a Thrush Infection
So, we know thrush is a yeast overgrowth. But the real question is why did it overgrow in the first place? Understanding the root cause is the key to not only getting rid of it but making sure it doesn’t come back.
Think of your skin’s natural ecosystem like a garden. A few weeds are normal and manageable. But when the conditions are just right, like too much water and not enough healthy plants to compete, those weeds can completely take over. Several factors can create this perfect storm for Candida to flourish, and it’s rarely just one thing.
Nipple Damage: The Open Door for Yeast
One of the biggest triggers for nipple thrush is any kind of damage to the skin. When your nipples are cracked, sore, or have even tiny, invisible breaks from a tough latch, it’s like leaving the front door wide open for yeast to march right in and set up shop.
A baby's latch is incredibly powerful. If it's not quite right, it can cause friction and trauma to that delicate tissue. This is especially common in the early days of breastfeeding, with one study showing that up to 88% of new parents had some form of nipple lesion. You can learn more about the research on nipple trauma and thrush here.
This damage creates a vulnerable spot where Candida, which normally lives harmlessly on your skin, can shift from a quiet resident to an aggressive invader.
The Role of Antibiotics and Your Microbiome
Have you recently been on antibiotics? Maybe for a C-section recovery, a stubborn UTI, or mastitis? While they are often essential, these medications can be a major setup for a thrush infection. Antibiotics are great at killing off bad bacteria, but they don't discriminate. They take out the good guys, too.
These beneficial bacteria are your body's built-in defense system against yeast. When they’re gone, Candida has no competition and can multiply unchecked. This is exactly why you might suddenly develop a thrush infection a week or two after finishing your prescription.
A weakened immune system plays a big part in your body’s ability to keep yeast in check. The postpartum period is already demanding, and factors like exhaustion, stress, and poor nutrition can lower your defenses, making you more susceptible to infections like thrush.
It’s also a good reminder that your overall health directly impacts your breastfeeding journey. For more on this, check out our guide on whether it's ok to breastfeed while sick.
Systemic Factors That Tip the Scales
Beyond direct nipple damage and medications, your overall health and environment play a massive role. Certain internal conditions can create a body-wide environment that encourages yeast to thrive.
Here are some of the most common systemic triggers:
- A Moist Environment. Yeast absolutely loves warm, damp places. Constantly leaking milk, wearing damp breast pads for too long, or even just sweaty bras create the perfect breeding ground for Candida right on your skin.
- High-Sugar Diet. Candida’s favorite food is sugar. A diet loaded with refined sugars and simple carbs can fuel yeast overgrowth in your gut and throughout your system, making skin infections more likely.
- Hormonal Changes. The huge hormonal shifts during the postpartum period can throw your body's microbial balance out of whack. For some, certain types of oral contraceptives can also be a contributing factor.
- Underlying Health Conditions. Certain medical issues can make you more prone to yeast infections. This includes conditions like diabetes (especially with uncontrolled blood sugar) and anemia.
By pinpointing which of these triggers might be affecting you, you and your healthcare provider can build a much more effective plan. one that not only treats the current infection but also helps stop it from ever coming back.
Recognizing the Symptoms in You and Your Baby
When it comes to nipple thrush, pain is often the first and loudest alarm bell. But this isn't the typical tenderness many people feel when they first start breastfeeding. Recognizing the unique signs in both you and your baby is the key to getting help fast.
Thrush pain tends to show up suddenly, sometimes weeks into what was a totally smooth breastfeeding journey. It's often described as a burning, itching, or stabbing sensation right on the surface of the nipple that doesn't let up once the feeding is over. For many, this is the biggest clue that something more than a simple latch issue is going on.
This intense pain can also feel like it's shooting from the nipple deep into the breast tissue. Some describe it as shards of glass or a hot poker, a feeling that can radiate into your back or shoulder and linger long after your baby has unlatched.
What to Look for on Your Nipples
Beyond just the pain, your nipples might look different. While some people have no visible signs at all, many notice distinct changes that point straight to a thrush infection. One of the classic visual symptoms is when the nipples and areolas turn a bright, almost glossy pink or red.
You might also spot other changes to the skin.
- Shiny or Flaky Skin: The skin on your nipple or areola might take on a shiny, almost Vaseline-like look, or it could become dry and flaky.
- A Rash with Tiny Blisters: Sometimes, a rash with very small blisters can pop up on the areola, signaling an inflammatory response to the yeast.
- Cracks at the Nipple Base: Small, incredibly painful cracks can form right where the nipple meets the areola, making every latch feel excruciating.
If you're dealing with any kind of breastfeeding discomfort, it's so important to get to the root of it. You can learn more in our guide on how to stop breastfeeding pain.
Spotting the Signs of Thrush in Your Baby
Because thrush is so easily passed back and forth, it’s critical to check your baby for symptoms at the same time. The infection often shows up as oral thrush in your baby’s mouth, which can make eating pretty uncomfortable for them.
The most telling sign is the presence of creamy white patches or dots inside your baby's mouth. These patches look a bit like leftover milk curds, but there’s a key difference. they don't wipe away easily. If you try to gently scrape them with a clean finger or soft cloth, the skin underneath might be raw and even bleed a little.
These white patches most commonly appear on the tongue, gums, inner cheeks, or the roof of the mouth. A baby's tongue is often white after a milk feeding, but with thrush, the whiteness is more cottage-cheese-like and persistent.
Your baby’s behavior can also be a major clue. Even if you can’t see obvious white patches, changes in their feeding habits can signal that their mouth is sore. Look for signs like unusual fussiness at the breast, pulling away and crying mid-feed, or making a clicking sound while nursing as they struggle to maintain a comfortable latch. In some cases, thrush can also cause a fiery red diaper rash that doesn’t clear up with typical diaper creams.
Symptom Checklist for Parent and Baby
Seeing the symptoms laid out side-by-side can make it easier to connect the dots. Here’s a quick comparison to help you assess what might be happening with both you and your little one.
| Symptom Area | Signs in the Parent | Signs in the Baby |
|---|---|---|
| Pain & Behavior | Sudden, severe nipple pain. Burning, shooting, or deep breast aches that continue after feeding. | Fussy or irritable at the breast. Pulls away while nursing. Clicking sounds during feeding. May refuse to nurse due to mouth soreness. |
| Visual Signs | Nipples are shiny, flaky, or bright pink/red. A rash with tiny blisters may be present. | Creamy white patches on the tongue, gums, or inside cheeks that do not wipe off. Fiery red diaper rash with pimple-like spots. |
If this checklist is hitting a little too close to home, it's a strong signal to reach out to both your healthcare provider and your baby's pediatrician. Treating both of you at the same time is the only way to effectively break the cycle and get back to comfortable, pain-free breastfeeding.
How Nipple Thrush Is Diagnosed and Treated
Getting to the bottom of nipple pain is the first step toward relief. Since so many different things can cause discomfort while breastfeeding, nailing down a correct diagnosis for nipple thrush is absolutely essential. The process usually kicks off with a simple, thorough conversation with your healthcare provider.
Your description of the classic symptoms, like that sudden, sharp, burning pain that sticks around long after a feed is over, is a massive clue. But sometimes, a quick visual check just isn't enough. Your doctor might need to take a swab from your nipple or your baby's mouth to send to a lab, confirming that Candida is indeed the culprit.
This step is so important because nipple pain is notoriously misdiagnosed. We have to rule out other common issues like bacterial infections or even vasospasms, where blood vessels in the nipple constrict and cause intense pain. Getting the right answer from the start means you get the right treatment and find relief faster.
Creating a Treatment Plan
Once thrush is confirmed, the golden rule is to treat both you and your baby at the same time. This is completely non-negotiable. If you only treat one of you, the infection will just ping-pong back and forth in a frustrating, seemingly endless cycle.
A typical treatment plan involves a two-pronged approach.
- For You: Your provider will likely prescribe a topical antifungal cream to apply directly to your nipples after each feeding. These creams get to work right on the skin to fight the yeast overgrowth where it started.
- For Your Baby: Your little one will usually get an oral antifungal medication. This is often a liquid gel or suspension that you’ll apply to the inside of their mouth several times a day.
It's vital to finish the entire course of medication for both of you, even if your symptoms seem to disappear after a few days. Stopping treatment too soon is like inviting the yeast to come right back.
The symptom recognition process usually follows a pretty clear path, starting with what you notice at home and leading to a professional diagnosis.
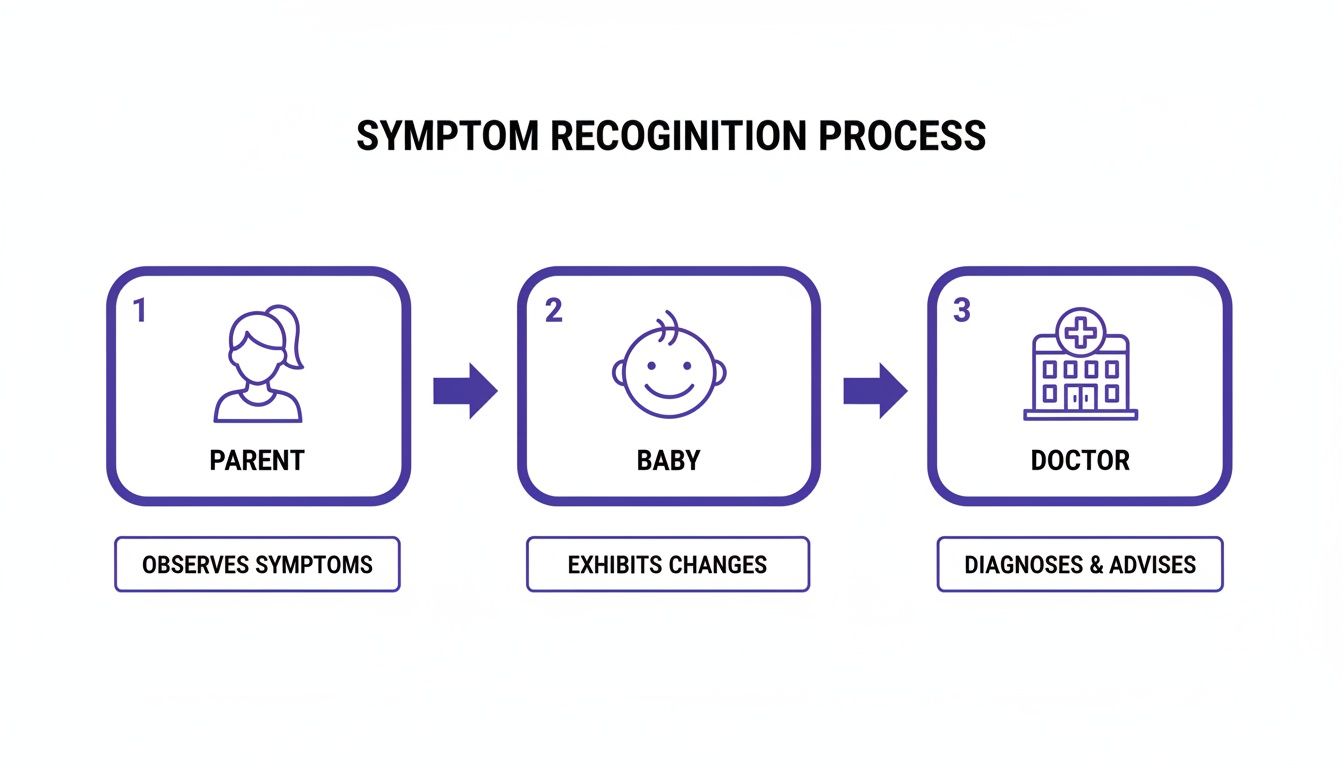
This visual really breaks it down: identifying symptoms in both the parent and the baby is the critical first step before you can get a medical opinion to confirm what's going on and get started on treatment.
When Topical Treatments Aren't Enough
Sometimes, a particularly stubborn or severe case of thrush needs a more powerful approach. If topical creams aren’t cutting it and your pain isn't improving, your doctor might prescribe an oral antifungal pill for you, like fluconazole. This medication works systemically, fighting the yeast infection from the inside out.
It's also worth noting how other factors can complicate the picture. For instance, recent studies using advanced PCR testing found that while bacteria are often present, Candida detection jumped to 54% in cases involving that specific burning nipple pain, really highlighting its role.
It is safe to continue breastfeeding while you and your baby are being treated for thrush. In fact, it's important to keep nursing to maintain your milk supply and prevent other issues like clogged ducts or mastitis. All standard treatments are designed to be safe for your nursing baby.
If you're hitting a wall trying to get a clear diagnosis or your treatment plan feels overwhelming, a lactation consultant can be an incredible ally. They can help spot underlying issues, like a poor latch, that might have contributed to the initial nipple damage and made you vulnerable to thrush in the first place. Check out our guide on what a lactation consultant does to see how they can support you. Their expertise can be a true game-changer in getting you back to comfortable, happy feeding.
Practical Ways to Prevent Thrush from Returning
Once you start treatment for nipple thrush, the goal shifts to preventing its comeback. Good hygiene is your best defense against another round, since Candida thrives in very specific, predictable environments. A few simple, practical steps can make your body a less welcoming home for yeast and break the cycle for good.
Many of these strategies come down to managing moisture and cutting off pathways for transferring yeast from one surface to another. Think of it as yeast-proofing your environment.
Maintaining Meticulous Hygiene
The foundation of thrush prevention is all about staying clean and dry. It might sound basic, but diligent handwashing is an incredibly powerful first step in stopping the spread of yeast.
Make sure you wash your hands with soap and water before and after every single feeding, every diaper change, and every time you apply antifungal cream. This simple routine is your front line against reintroducing yeast to your nipples or your baby's mouth.
Beyond your hands, you’ll want to pay close attention to anything that comes into contact with your breasts or your baby.
- Bras and Breast Pads. Wash any bras, reusable breast pads, or clothing that touches your nipples in hot water. To kill any stubborn yeast spores, dry them completely on a high heat setting or, even better, in direct sunlight.
- Disposable Pads. While you’re actively treating thrush, it’s a good idea to switch to disposable breast pads. The moment they feel even slightly damp, change them out to keep your skin as dry as possible.
- Baby's Items. Anything that goes into your baby's mouth, like pacifiers, bottle nipples, and teething toys, needs daily attention.
Sterilizing Feeding and Pumping Equipment
If you use a breast pump, meticulous cleaning is absolutely non-negotiable. Yeast can easily hide out in the tiny nooks and crannies of pump parts, creating a sneaky source of reinfection.
During a thrush outbreak, any pump parts that touch you or your milk should be sterilized at least once a day. You can do this by boiling them in water for 5 to 10 minutes or by using a microwave steam bag designed for this purpose. After sterilizing, let the parts air-dry completely on a clean paper towel before putting them away.
Keeping things dry is just as important as keeping them clean. After a feeding, let your nipples air-dry for a few minutes before putting your bra back on. This small step helps reduce the trapped moisture that yeast loves.
This daily sterilization routine should also apply to any bottles or pacifiers your baby uses. It might feel like a lot of extra work, but it’s one of the most effective ways to ensure you aren’t accidentally re-exposing yourself or your baby to the fungus you’re working so hard to get rid of.
Simple Nipple Care Tips
A few small tweaks to your daily routine can make a huge difference in keeping your nipples healthy and less prone to another infection. The goal is simple: create an environment where yeast just can’t get a foothold.
Focus on keeping the area dry and clean all day. If you leak milk, changing your breast pads often is crucial. A damp pad pressed against your skin is the perfect breeding ground for Candida.
Some people also find that a mild rinse after feedings can be helpful. A simple solution of one cup of water mixed with one tablespoon of white vinegar can help restore your skin's natural pH balance, making it less hospitable to yeast. Just remember to always pat your nipples completely dry afterward, before you apply any prescribed creams or get dressed. These practical tasks are key to understanding what causes nipple thrush to return and how to stop it.
Where to Find Breastfeeding Support and Guidance
Navigating nipple thrush is not just physically painful. it's emotionally draining. But you absolutely do not have to figure this out on your own. Finding the right professional help is one of the most important steps you can take to get relief and feel confident about breastfeeding again.
The intense, shooting pains from thrush can make you want to give up entirely, which is why having an expert in your corner is so essential. A professional can confirm what’s really going on, help you create a treatment plan that actually works, and pinpoint any underlying issues that opened the door to the infection in the first place.
The Vital Role of a Lactation Consultant
An International Board Certified Lactation Consultant (IBCLC) is a healthcare professional who specializes in all things breastfeeding. Think of them as your personal guide through the ups and downs of nursing. When you’re dealing with something as tricky as thrush, their expertise is invaluable.
Here are a few key ways an IBCLC can help:
- Confirm the Cause: They are trained to tell the difference between the unique pain of thrush and other common issues like a poor latch or a bacterial infection. This is critical for getting the right treatment from the start.
- Improve Your Latch: If nipple damage was the root cause of your thrush infection, an IBCLC can work with you to correct your baby’s latch. This prevents more trauma and gives your skin a chance to finally heal.
- Develop a Care Plan: They’ll partner with you to create a comprehensive plan, offering clear guidance on medications, hygiene practices, and comfort measures to see you through the infection.
Finding solid support isn't just about treating thrush. it's about protecting your overall wellbeing during what can be a really challenging time. An IBCLC brings both clinical knowledge and emotional reassurance, a powerful combination when you’re feeling completely overwhelmed.
How to Connect with Vetted Professionals
Knowing you need help is one thing, but finding the right person is another. Thankfully, platforms like Bornbir make it much easier to connect with vetted perinatal professionals in your area or for virtual appointments.
Instead of falling down an internet rabbit hole for hours, Bornbir lets you find and compare lactation consultants, doulas, and other specialists who fit your exact needs. You can read real reviews from other parents, check credentials, and see their availability all in one place. For more ideas on building your team, you can learn more about postpartum support services in our detailed guide.
The right support can be a game-changer. It turns a stressful, painful experience into a manageable problem with a clear solution, empowering you to continue your breastfeeding journey with confidence.
Whether you need someone to come to your home to check your baby’s latch or just want a virtual consultation to talk through your symptoms, having a simple way to find trusted support is key. You don’t have to push through the pain and frustration of nipple thrush alone. Reaching out is a sign of strength, and it’s the fastest way back to comfortable, enjoyable feedings.
Common Questions About Nipple Thrush
When you're dealing with the pain and confusion of nipple thrush, it's natural to have a million questions running through your mind. Let's get you some quick, clear answers to the most common concerns.
Can I Still Breastfeed with Nipple Thrush?
Yes, you can and you absolutely should. Stopping breastfeeding can actually make things worse by causing blocked ducts or even mastitis, so it's important to keep nursing to maintain your milk supply.
Plus, the medications prescribed for thrush are safe for your baby. Think of continuing to breastfeed as part of the treatment plan for both of you. it helps you heal without interrupting your baby’s feeding.
How Long Does Treatment Take to Work?
Most people start feeling some real relief within 2 to 3 days of starting medication. But, and this is a big one, you have to finish the entire course of medication your doctor prescribed.
It can be tempting to stop once you feel better, but that's a recipe for a quick comeback. Finishing the full treatment is the only way to be sure you've knocked out the Candida for good.
The key to successful treatment is consistency. Even when symptoms improve, the underlying fungal spores may still be present. Completing the full medication course is the best way to ensure they are gone for good.
Can Nipple Thrush Come Back?
Unfortunately, yes. Thrush is notorious for making a return appearance, especially if the original risk factors haven't been sorted out.
This is exactly why all those prevention tips are so crucial. Being diligent about hygiene, changing your breast pads frequently to stay dry, and sterilizing your pump parts and bottles are your best defenses. If you find yourself in a frustrating cycle of recurring infections, it's time to talk with your provider to dig a little deeper for hidden triggers.
Should I Change My Diet to Help with Thrush?
Some parents find that adjusting their diet helps them feel more in control. Since yeast thrives on sugar, cutting back on sugary foods and refined carbs can make your body a less welcoming place for Candida.
While a diet change alone won't cure thrush, eating a balanced, nutrient-rich diet gives your immune system the fuel it needs. A stronger immune system is better at keeping yeast in check, which can help prevent flare-ups down the road.
Navigating breastfeeding challenges is easier with the right support. Bornbir connects you with vetted, top-rated lactation consultants, doulas, and other perinatal professionals who can provide expert guidance in person or virtually. Find the help you need to breastfeed confidently at https://www.bornbir.com.
